Posted on Nov 4, 2013 in Original Article |
Matthew Skomorowski, MD1, Kim Jordan, MD, FACP1, Kevin Schroeder, MD1, John O. Elliott, PhD, MPH1
1Department of Medical Education, Riverside Methodist Hospital, Columbus, USA
Corresponding Author: mskomor2@ohiohealth.com
Journal MTM 2:3:21–26, 2013
doi:10.7309/jmtm.2.3.5
Background Physician use of the iPad as a clinical and educational tool has increased since its release in 2010. Few studies have assessed resident perception of the iPad as an educational and daily clinical tool.
Aims This study evaluates residents’ perceptions of the iPad’s clinical and educational utility, and examines differences of perceived value between medicine-based and surgical-based residents.
Methods During the academic year 2011–2012, all residents (n = 119) utilized a 16GB iPad. Opinions on clinical utility and educational value were assessed by survey at year’s end. Responses were dichotomized as often /always vs. never/rarely/sometimes for comparison analysis via Chi-square tests.
Results One-hundred-and-two (86%) residents participated. The iPad received low marks for daily clinical utility (14.7%) and efficiency in documentation (7.8%). It was most valued for sourcing articles outside the hospital (57.8%), and as a research tool (52%). Medical and surgical residents’ opinions differed regarding perceived value for educational utility (41.7% vs. 6.7%, p ≤ 0.001), viewing results and use as an Evidence-based Medicine resource (38.9% vs. 16.7%, p = 0.037), recommendation to a colleague (58.3% vs. 36.7%, p = 0.053), and facilitation of patient care (45.8% vs. 23.3%, p = 0.045).
Conclusion Residents in this study did not attribute high value to the iPad as a clinical rounding or educational tool. Additionally significant differences existed between medical and surgical residents’ perceived value of the iPad’s utility. Institutions should consider these differences and address connectivity and support issues before implementing iPad programs across all disciplines.
Posted on Nov 4, 2013 in Letter to the Editor |
Chris Smith, MBBCh, MSc1,2, Uk Vannak, BN1, Ly Sokhey, BM1, Melissa Cockroft, BA, MA1
1Marie Stopes International Cambodia (MSIC); 2Department of Population Health, London School of Hygiene and Tropical Medicine (LSHTM), London, UK
Corresponding Author: chris.smith@mariestopes.org.kh
doi:10.7309/jmtm.2.3.6
We concur with the mHealth operational challenges in Cambodia identified in Bisit Bullen’s perspective piece1. We would like to share our experiences with MOTIF (MObile Technology for Improved Family Planning); a project to design and evaluate a mobile phone-based service to support post-abortion family planning (PAFP) clients accessing services at Marie Stopes International Cambodia’s (MSIC) clinics.
Posted on Nov 3, 2013 in News |

The Editorial Board at the Journal of Mobile Technology in Medicine is proud to present Volume 2, Issue 3, published in November 2013. Mobile technology in Medicine is a rapidly developing area, and we hope to continue accelerating research in the field. We look forward to your submissions for Issue 4.
Posted on Oct 29, 2013 in News |
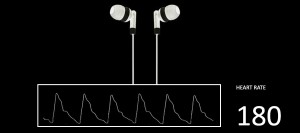
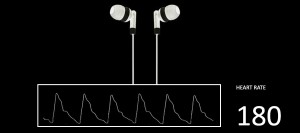
Your run-of-the-mill earphones could be the latest innovation in mobile health technology. In the past, music has gotten pulses racing, now with health, it seems we can measure how much by. The Kaiteki Institute in Japan and Bifrostec has been developing technology to turn earphones into pulse rate monitors via special software algorithms.
This technology works by utilising the pressure change in the enclosed ear caused by pulsating arteries when earphones are worn. This pressure change occurs at roughly 1Hz and can be detected by earbuds functioning as microphones. Since earphones do not always make a completely enclosed space and measurements can be influenced by ambient noise, the companies have created unique signal processing technologies to combat these issues.
Given the rise of the “Quantified Self” movement, many fitness tracking devices and apps have hit the market. One possible utilisation of this technology could be a simple pulse tracker for those who prefer to run while listening to music with one less gadget to carry. The companies are also developing “at home” medical vital sign monitoring equipment for the future based on similar principles.
Source:
http://www.bifrostec.co.jp/english/index.html
http://www.kaiteki-institute.com/research/activities/2013/20130729.html
http://techon.nikkeibp.co.jp/english/NEWS_EN/20131025/311441/
Posted on Oct 27, 2013 in News |
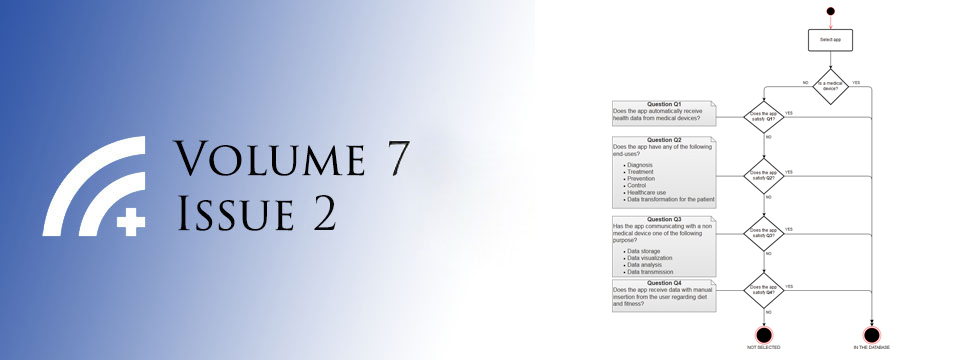
The FDA guidelines which were recently published have required FDA approval for certain types of apps and mobile attachments which are essentially designed to function as medical devices which would have otherwise required FDA clerance. Here are some FDA approved programs which are a great model for future devices/apps.
Posted on Oct 15, 2013 in News |
Sotera Wireless recently announced that one of the company’s key products, the continuous non-invasive blood pressure monitor (cNIBP), has cleared the FDA regulatory process. This means that continuous, beat-to-beat, cuff and invasive catheter less blood pressure measurements are one step closer to hitting hospital floors.
This technology is part of the ViSi Mobile patient monitoring system that is being developed by the San Diego based company. Once released, the wrist worn device will allow for the continuous measurement of all core patient vital signs including blood pressure, heart rate, ECG, oxygen saturation, respiratory rate and even skin temperature. Sotera claims that the accuracy of the devices can match those offered by the systems used in Intensive Care Units, citing studies that show blood pressure accuracy is claimed to be within a range of 5mmHg as compared to invasive arterial line monitoring.
Wireless monitoring technology could prove to be revolutionary in healthcare as it has the potential to dramatically reduce the workload on healthcare staff, where routine measurements of vital signs take considerable time. The wireless nature of the system would also allow computer/mobile based access to the vital signs, alleviating the need to “hunt for the patient charts” during the daily medical ward round.
Dr Bob Murad, Co-founder of Sotera, said ““Hospitals are now safer, gentler places. With continuous monitoring of all vital signs, now including cuffless and continuous blood pressure, hospitals can be confident that deterioration in a patient’s condition will not go unnoticed for hours at a time between periods of observation. No longer will healing patients have to endure sleep interruptions in order to document that all is well.”
Press Release: http://www.soterawireless.com/wp-content/uploads/2013/10/new_cNIBP_clearance_PR010-100913Final.pdf