Posted on Dec 5, 2013 in Conference |
Thomasena O’Byrne 1, Deborah Nyirenda 3, Rachel Perrin 2, Sara Marshall 2, Marije Geldof 7, Sarah Bar-Zeev 5, Norman Lufesi 6, Eltas Nyirenda 6, Queen Dube 3,4, Naor Bar-Zeev 3, Linda Glennie 2, Elizabeth Molyneux 4, Robert Heyderman 3,5, Nicola Desmond 3,5
1Action Meningitis, Meningitis Research Foundation, Malawi; 2Meningitis Research Foundation, UK; 3Malawi Liverpool Wellcome Trust Clinical Research Programme, Malawi; 4College of Medicine, Malawi; 5Liverpool School of Tropical Medicine, UK; 6Ministry of Health, Malawi; 7D-Tree International, Malawi
Journal MTM 2:4S:2–3, 2013
DOI: 10.7309/jmtm.2.4S.2
Abstract
Hospital-based studies suggest that late presentation at tertiary level is a driving factor for mortality from severe febrile illness in resource-poor contexts. Recent research into health seeking pathways in Malawi identified primary level barriers linked to service provision and misdiagnoses. In Malawi an Emergency Triage, Assessment and Treatment (ETAT) package, approved by the World Health Organisation (WHO) has been introduced at tertiary level and is being rolled out to district and primary clinics. mHealth technologies are likely to sustain quality in implementing clinical protocols, particularly when community-based health providers with limited formal training are increasingly working to offset primary level staff shortages.
We aimed to develop and evaluate feasibility and acceptability of a prototype primary care level intervention to improve triage, assessment and referral of children with severe illness in Blantyre and to investigate whether this facilitates systematic and timely recognition and response to severe illness.
All paediatric cases within five primary clinics in urban Blantyre were triaged and assigned Red for Emergency, Amber for Priority and Green for Queue using the mHealth triage algorithm. Phones were assigned to triage, to clinicians and the A&E department within the local tertiary, referral hospital (Queen Elizabeth Central Hospital (QECH)) for monitoring patient referrals.
We conducted a rigorous evaluation using a combination of quantitative and qualitative approaches, both pre- and post and, using the phone as a monitoring tool, in parallel to the intervention.
Seventy-four healthcare staff were trained across five urban primary clinics. A total of 41,358 patients were assessed using the mHealth triage algorithm from December 2012 to May 2013, of whom 1.56% were referred to QECH. Rates of concordance between triage and clinician assessment showed a good level of agreement above chance (Kappa value = 0.71). Pre- and post-Patient Journey Modelling tools identified positive changes in patient flows. Overall patient and health worker satisfaction was high with indirect impact on quality of clinical assessment amongst health workers based at intervention clinics but not directly involved in the intervention.
This study has shown that mHealth technologies have the potential to improve primary level health services in resource-poor contexts with high patient numbers and overburdened health staff. Working in collaboration with the Ministry of Health the data we present will inform the development of a cluster-randomised trial to rigorously evaluate the role of mHealth in the implementation of ETAT. This will aid policy decisions around ETAT implementation at primary health level.
Posted on Dec 1, 2013 in News |
Crowd-sourcing has become quite popular method of raising capital for up and coming startups and the mHealth sector is no stranger to the concept, with a project recently having reached funds on Indiegogo for Dextrus: the open source robotic prosthetic hand.
The campaign reached its $64000 goal in just over a month with sponsors donating around an additional $8000 in excess.
The company has pledged to use the funds to create a viable prosthetic arm that can be sold for under $1000. It hopes to publish the designs of the prosthetic as an open-source project with no patents so that other companies can develop on it and further improve on the concept. Their focus also extends to the developing world where import taxes impose a significant cost burden on such devices.
Dextrus is currently already being used in its prototype form by Chef Liam Corbett, who lost his right arm as a complication of meningitis. Some of you may have already sampled food prepared by robot hands.
Source: http://www.indiegogo.com/projects/the-open-hand-project-a-low-cost-robotic-hand

Posted on Nov 4, 2013 in Editorial |
Barbara A. Binzak Blumenfeld, PhD, JD1, William A. Garvin, JD1
1Counsels for Buchanan Ingersoll & Rooney PC
www.bipc.com
Journal MTM 2:3:1–3, 2013
10.7309/jmtm.2.3.1
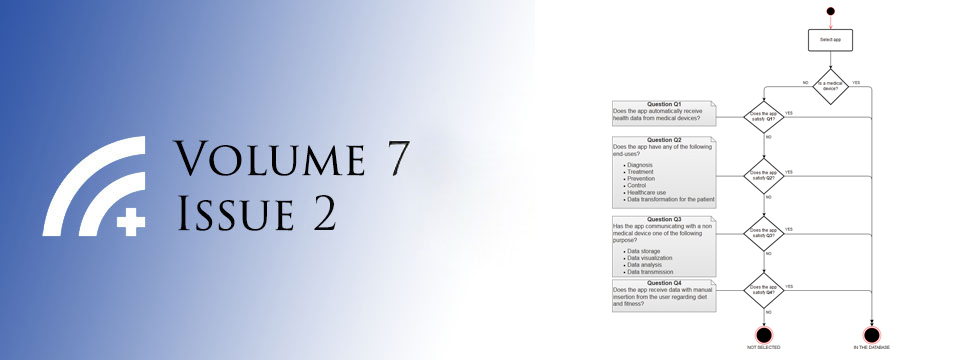
In a previous issue of the Journal of Mobile Technology and Medicine, we provided an overview of the regulation in the United States of mobile health (“mHealth”) and mobile medical applications (“mobile medical apps”).1 On September 25, 2013, the United States Food and Drug Administration (“FDA”) released a Final Guidance for Industry and FDA Staff on Mobile Medical Applications (“Final Mobile Medical Apps Guidance” or “Final Guidance”).2 While the basic framework for regulating mobile medical apps in the United States has remained unchanged from our previous article, the new guidance provides further clarity that should be carefully considered by those developing mobile medical apps.
Posted on Nov 4, 2013 in Editorial |
Chandrashan Perera 1, Rahul Chakrabarti 1,2
1Chief Editor, Journal of Mobile Technology in Medicine; 2Centre for Eye Research, University of Melbourne, Melbourne, Australia
Journal MTM 2:3:4–6, 2013
10.7309/jmtm.2.3.2
Introduction
Mobile devices are uniquely positioned to make a significant contribution to medical imaging. Portability, computing power, accessibility and built in internet connectivity are well described advantages of mobile devices.1 There is a growing body of research which supports the use of mHealth technologies for imaging, and a number of novel uses are described in the literature.
Posted on Nov 4, 2013 in Original Article |
Debra A. Goff, PharmD, FCCP1, Kim Hawksworth, RPh1, Julie E. Mangino, MD, FSHEA2,3
1Department of Pharmacy, The Ohio State University Wexner Medical Center, OH, USA; 2Division of Infectious Diseases in the Department of Internal Medicine, The Ohio State University, OH, USA; 3Department of Clinical Epidemiology, The Ohio State University Wexner Medical Center, OH, USA
Corresponding Author: debbie.goff@osumc.edu
Journal MTM 2:3:15–20, 2013
10.7309/jmtm.2.3.4
Background: Research addressing how physicians utilize apps is growing, however, there is little data to show apps improve patient outcomes.
Aims: Develop an iPhone/iPad app to educate physicians on management of Staphylococcus aureus bacteremia. Secondary goals include assessing app utilization and patient outcomes pre/post implementation.
Methods: A web-based app STAB-IT™ (S. aureus bacteremia is terrible) was developed and provides: hospital specific epidemiology, microbiology, diagnosis, management, antibiotics, patient education and quiz. Learning outcome was measured by a pre/post quiz. App use was prospectively monitored using Google analytics and outcomes were retrospectively collected. Patients were eligible if admitted between September 2010 to May 2011 n =222 (i.e. pre-STAB-IT™) and September 2011 to May 2012 n=191 (i.e. post STAB-IT™) with S. aureus bacteremia. Data included age, blood cultures, vancomycin levels, negative blood cultures prior to discharge, infectious diseases consultation, time to consultation, length of stay, mortality, and hospital re-admissions.
Results: Physician knowledge of managing patients with S. aureus bacteremia significantly improved after learning how to navigate STAB-IT™ (50.2% vs. 86.6% p=0.0001). Mean utilization was 50 visitors / month, 217 (61.5%) new visitors and 136 (38.5%) returning visitors. No significant differences were seen in clinical outcomes measured in the post group.
Conclusion: Learning how to navigate a web-based app STAB-IT™ improved physicians knowledge of managing patients with S. aureus bacteremia. Larger studies over a longer time period are needed to further define the relationship between app use and patient outcomes for this common clinical condition.
Posted on Nov 4, 2013 in Original Article |
Mia L. van der Kop MSc1,2, Jasmina Memetovic, MSc3, Kirsten Smillie, MA4, Jesse Coleman, MA5, Jan Hajek, MD3, Natasha Van Borek MA4, Darlene Taylor, MSc4,6, Kadria Alasaly, MD4, James Johnston, MSc, MD4, Richard T. Lester, MD3,4, Fawziah Marra, PhD7
1University of British Columbia Centre for Disease Control, Vancouver, Canada; 2Department of Public Health Sciences, Karolinska Institutet, Stockholm, Sweden; 3Department of Medicine, University of British Columbia, Vancouver, Canada; 4Clinical Prevention Services, British Columbia Centre for Disease Control, Vancouver, Canada; 5Wits Reproductive Health & HIV Institute, Johannesburg, South Africa; 6School of Population and Public Health, University of British Columbia, Vancouver, Canada; 7Faculty of Pharmaceutical Sciences, University of British Columbia, Vancouver, Canada
Corresponding Author: miavanderkop@gmail.com
Journal MTM 2:3:7–14, 2013
10.7309/jmtm.2.3.3
Background: Successful treatment of latent tuberculosis infection (LTBI) is critical to reduce the impact of tuberculosis (TB). The purpose of this study was to determine the feasibility of adopting the WelTel text-messaging intervention, proven to be effective in improving HIV treatment adherence, for use in LTBI care.
Aims: (1) Determine prevalence of mobile phone ownership, text-message use, and patient attitudes towards receiving text messages from the clinic. (2) Determine the technological feasibility of the WelTel intervention, and (3) patient and healthcare provider acceptability of the service.
Methods: We conducted a cross-sectional descriptive survey of patients attending a provincial TB clinic and a pilot study in which patients initiating treatment for LTBI received the intervention for 12 weeks.
Results: Clinic survey: Of 82 participants who completed the survey between September and December 2011, 68 owned a mobile phone and 58 used text messaging weekly. Participants were receptive to receiving text-message communication from the clinic (n = 80). Pilot intervention study: Of 16 patients who received the intervention, 14 completed the study. Using software to deliver the intervention was feasible. The greatest participant-perceived benefit was that it enabled them to report side-effects quickly (n = 6); the greatest participant-perceived barrier was cost (n = 3).
Conclusion: The majority of patients in this study population had the means to communicate with their healthcare providers via text-messaging and were receptive to doing so. The intervention was well-received by participants and the healthcare provider. A randomized controlled trial is underway to determine the intervention’s effectiveness to increase LTBI treatment adherence.