Patients’ Attitudes Towards Text Messages about HIV and Hepatitis C Screening
Patients’ Attitudes Towards Text Messages about HIV and Hepatitis C Screening
Julika Kaplan, MD1, Haley Marek, BS2, Monisha Arya, MD, MPH1,3
1 Department of Medicine, Baylor College of Medicine, Houston, TX, USA
2 School of Medicine, Baylor College of Medicine, Houston, TX, USA
3 Center for Innovations in Quality, Effectiveness and Safety, Michael E. DeBakey VA Medical Center, Houston, TX, USA
Corresponding author: julika.kaplan@bcm.edu
Journal MTM 7:2:51–54, 2018
Background: Despite the prevalence of HIV and hepatitis C virus (HCV), many people in the United States have never been screened for these infections. Mobile phones could educate patients about screening recommendations and “nudge” them to request screening from their physicians. There is a need for studies to understand patients’ perspectives on this campaign strategy.
Aims: The purpose of this pilot study is to describe patients’ attitudes towards text messages that educated them about HIV and HCV and “nudged” them to discuss screening recommendations with their physicians.
Methods: In 2016 and 2017, patients in primary care clinics in Houston, Texas were recruited to participate in text message studies promoting HIV and HCV screening. Participants were sent either HIV, HCV, or control text messages prior to their individual primary care appointments. After the appointment, research staff called the participants and conducted evaluation surveys to determine whether they enjoyed receiving health-related text messages and to elicit their opinions about the specific content of the messages.
Results: The majority of our participants appreciated the text messages, specifically because they provided valuable health information that was unfamiliar to the patients and prompted them to discuss HIV and HCV screening with their physicians.
Conclusion: Our pilot study demonstrated that the majority of patients enjoyed receiving text message-based “nudges” because they helped them overcome barriers to healthy behavior and may have improved patient-physician communication. These findings are important because this strategy can improve screening rates in primary care for infections such as HIV and HCV.
Keywords: Text Messaging, Hepatitis C, HIV Infections, Mobile Health, Pilot Projects
Introduction
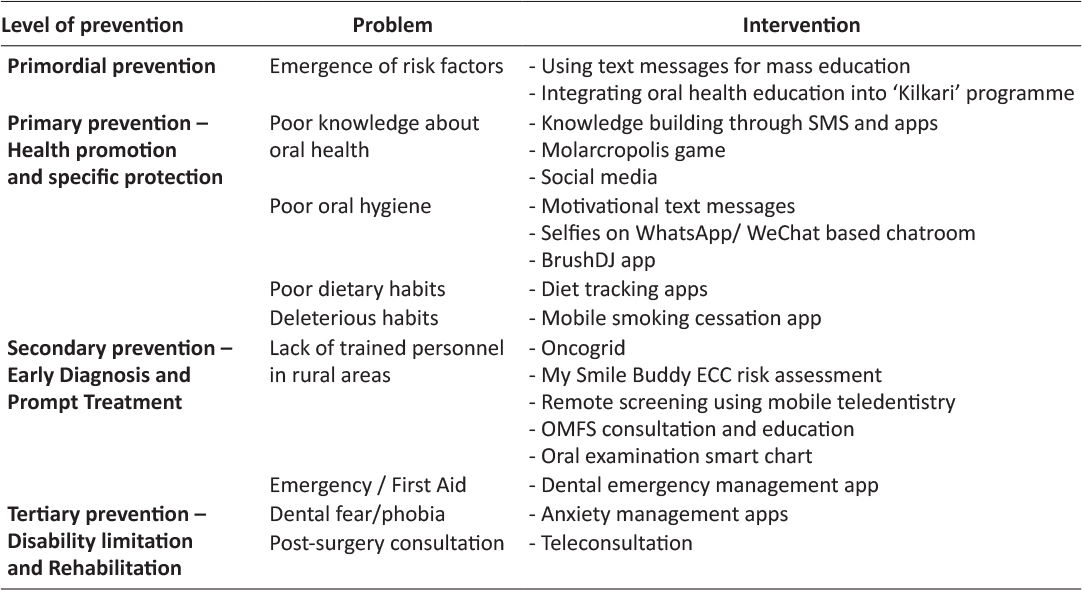
Despite the prevalence of HIV and hepatitis C virus (HCV), many people in the United States have never been screened for these infections.1,2 This is partially due to a lack of physician awareness of national screening recommendations.3,4,5 Screening and early detection are critical to improving health outcomes for HIV and HCV, so strategies to increase routine screening in healthcare are necessary.6,7 While improving physician awareness of screening recommendations could be one approach, a patient-focused strategy may be to use mobile health (mHealth) technology to provide targeted health information directly to patients. Mobile phones, specifically, could educate patients about screening recommendations and “nudge” them to actively engage in their healthcare.8 In the case of health, “nudging” involves using interventions to help people overcome the barriers that may be limiting their ability to obtain optimal healthcare.9 We developed text message campaigns in which we educated patients about HIV and HCV and “nudged” them to discuss screening with their physicians. The purpose of this pilot study is to describe patients’ attitudes towards these HIV and HCV text messages.
Methods
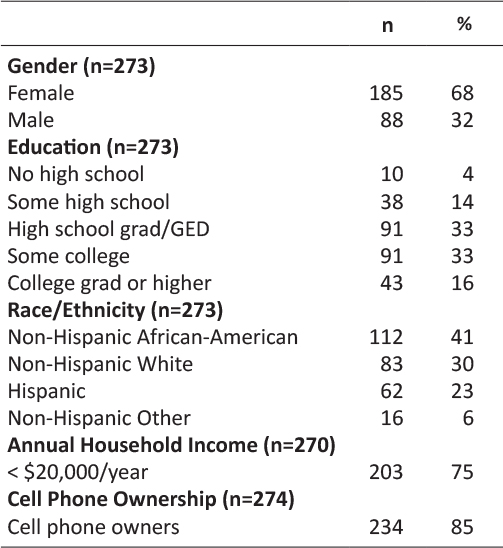
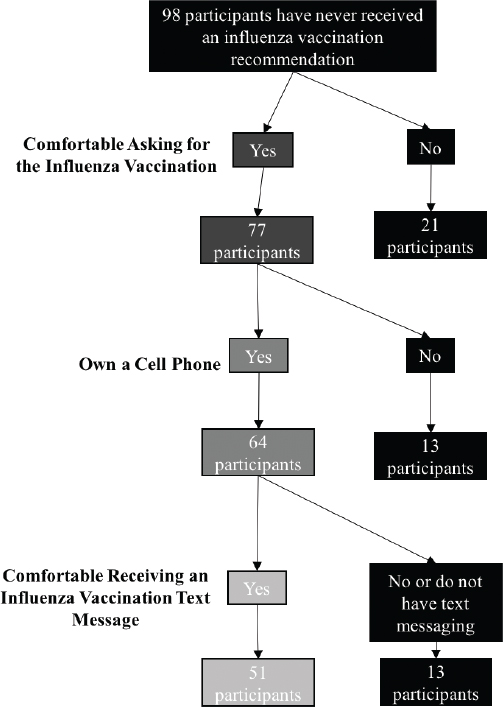
In 2016 and 2017, patients in primary care clinics in Houston, Texas were recruited to participate in mHealth text message studies promoting HIV and HCV screening. During the consent process, patients were informed that they would receive a message either about HIV, HCV, or a different health topic. Patients who participated had mobile phones, used text messaging, and provided informed consent. Participants in the HIV study were sent an HIV text message or a control text message, and participants in the HCV study were sent an HCV text message or a control text message. Each message included a one-sentence fact about HIV or HCV and a prompt encouraging participants to talk to their physicians about screening. The messages were sent within the hour prior to their individual primary care appointments. After the appointment, research staff called the participants and conducted evaluation surveys to determine whether they enjoyed receiving health-related text messages and to elicit their opinions about the specific content of the messages. The Baylor College of Medicine Institutional Review Board approved these studies.
Results
For both our HIV and HCV campaigns, we found that the majority of participants enjoyed receiving text messages with health information. Our post-text evaluation surveys provided insight into why our participants did or did not enjoy receiving health-related messages before their appointments with their physicians.
Out of our 12 HIV text message recipients, 11 (92%) enjoyed receiving a health-related text message, while one (8%) did not. Those who enjoyed receiving the message cited the following reasons: seven (64%) appreciated a health reminder, two (18%) felt that the message provided valuable information relevant to their health, and one (9%) believed that texting was more effective than calling as a communication method. A participant who benefitted from the reminder about HIV testing stated, “I liked it because it reminded me to ask my doctor about the HIV test.” Another acknowledged that the text instructed her “to do something that [she] otherwise wouldn’t have asked.” One of the participants who valued the information he received said the message “[kept him] on point” and let him know that he could get an HIV test “without setting a special appointment.” Another participant expressed her belief that “[HIV] is a disease that everyone should be on top of.” Finally, there were several participants who found the text message useful but still confessed that it was “alarming” or “a little disturbing” because people do not normally “send a text message out of the blue about something like [HIV].” On the other hand, the single participant who did not enjoy receiving our HIV text message was concerned that her confidentiality could be breached if a friend saw her phone: “It was a personal message but it was to my phone. I’m okay with it… but it could be a problem… someone snooping could cause a problem.”
Out of the 25 participants who received text messages about HCV, 22 (88%) enjoyed receiving a health-related text message, while two (8%) did not and one (4%) felt neutral. Those who enjoyed receiving the message cited the following reasons: 14 (64%) felt that the message provided valuable information relevant to their health, seven (32%) appreciated a health reminder, and one (5%) believed that receiving the text message was easy and convenient. One participant who was grateful that the text message prompted her to discuss HCV with her physician stated: “At appointments, it’s hard to remember what you want to bring up with your doctor. This text can function as a jumping off point for initial discussion.” Two other participants felt that the text message provided valuable information about their health; one said the message “pertained to an issue most people don’t know about,” and another said he “never thought about a hepatitis C test at [his] age.” One participant who did not enjoy receiving the text message said he “didn’t understand the purpose” of the text message.
Discussion
In this pilot study, we encouraged participants to discuss HIV and HCV screening with their physicians by sending them informative text messages with cues to action prior to their appointments. We learned that participants appreciated our text messages because they provided valuable health information and prompted them to discuss HIV and HCV screening with their physicians. However, despite the consent process, we also found that one patient had concerns about receiving health information on her cell phone that she considered alarming and another patient did not understand the purpose of the text message campaign.
The limitations of this study include a small sample size, which may hinder generalizability. However, this pilot study provides proof of concept for using text messages as an intervention to promote HIV and HCV screening. Another potential limitation is social desirability bias, or participants’ tendency to give responses that will satisfy the research staff. We attempted to mitigate this limitation by emphasizing before participants completed the evaluation survey that there were no correct answers and that their participation would not impact their medical care.
People face many barriers that may negatively impact their ability to make decisions that are good for their health. Examples of these barriers include limited awareness of medical topics, difficulty remembering to ask their providers certain questions, or fear of receiving an unwanted diagnosis, particularly in the case of chronic infections such as HIV and HCV. A “nudge” is a policy change or intervention that helps people overcome these barriers, thereby making it easier for people to act in their own best interest and make healthy decisions. Our study demonstrates that the majority of patients enjoyed receiving a text message-based “nudge” because it helped them overcome two of their most significant barriers: lack of information about screening recommendations and difficulty remembering health information. These findings are important because they can improve screening rates for asymptomatic yet treatable diseases such as HIV and HCV in primary care. Larger studies are needed to confirm our findings and determine the impact on screening rates.
Acknowledgements
The authors would like to thank John Benjamin Kellogg, Jessica Lee, Sharon Joy, and Stephen Manning for their contributions to data collection. The HIV-related work was supported by the National Institute of Mental Health of the National Institutes of Health under Award Number K23MH094235 (Principal Investigator: Arya). This work was also supported in part by the Center for Innovations in Quality, Effectiveness and Safety (#CIN 13-413) of the Michael E. DeBakey Veterans Affairs Medical Center in Houston. The views expressed in this article are those of the authors and do not necessarily represent the views of the National Institutes of Health or of the US Department of Veterans Affairs.
References
1. Dailey AF, Hoots BE, Hall HI, Song R, Hayes D, Fulton Jr P, Prejean J, Hernandez AL, Koenig LJ, Valleroy LA. Vital Signs: Human Immunodeficiency Virus Testing and Diagnosis Delays—United States. Morbidity and Mortality Weekly Report. 2017 Dec 1;66(47):1300–1306. ![]()
2. Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Teo CG, Jewett A, Baack B, Rein DB, Patel N, Alter M. Recommendations for the Identification of Chronic Hepatitis C Virus Infection Among Persons Born During 1945–1965. Morbidity and Mortality Weekly Report: Recommendations and Reports. 2012 Aug 17;61(4):1–32. ![]()
3. Zheng MY, Suneja A, Chou AL, Arya M. Physician Barriers to Successful Implementation of US Preventive Services Task Force Routine HIV Testing Recommendations. Journal of the International Association of Providers of AIDS Care. 2014 May;13(3):200–205.
4. Falade-Nwulia O, McAdams-Mahmoud A, Irvin R, Niculescu A, Page KR, Mix M, Thomas DL, Sulkowski MS, Mehta SH. Primary Care Providers Knowledge, Attitude and Practices Related to Hepatitis C Screening and Treatment in the Oral Direct Acting Antiviral Agents Era. Journal of Community Medicine & Health Education. 2016 Oct;6(5).
5. Thomson M, Konerman MA, Choxi H, Lok AS. Primary Care Physician Perspectives on Hepatitis C Management in the Era of Direct-Acting Antiviral Therapy. Digestive Diseases and Sciences. 2016 Dec 1;61(12):3460–3468. ![]()
6. Moyer VA. Screening for HIV: US Preventive Services Task Force Recommendation Statement. Annals of Internal Medicine. 2013 Jul 2;159(1):51–60. ![]()
7. Younossi Z, Blissett D, Blissett R, Henry L, Younossi Y, Beckerman R, Hunt S. In an Era of Highly Effective Treatment, Hepatitis C Screening of the General Population of the United States for Hepatitis C Should be Considered. Liver International. 2017 Jul 18:38(2):258–265. ![]()
8. Arya M, Kumar D, Patel S, Street Jr RL, Giordano TP, Viswanath K. Mitigating HIV Health Disparities: The Promise of Mobile Health for a Patient-Initiated Solution. American Journal of Public Health. 2014 Dec;104(12):2251–2255. ![]()
9. Thaler RH, Sunstein CR. Nudge: Improving Decisions about Health, Wealth, and Happiness. New Haven, CT. Yale University Press; 1999.
Read More