Mobile Applications for Stroke Prevention: A Survey of Physicians’ Perspectives
Douglas Halket, BS1, Jonathan Singer, MA2, Clotilde Balucani, MD, PhD3, Dimitre Stefanov, PhD3, Steven R. Levine, MD, FAHA, FAAN, FANA4
1SUNY Downstate College of Medicine, MSC, Brooklyn, NY; 2University of Nevada, Reno, Clinical Psychology, MSS, Reno, NV, 3SUNY Downstate Medical Center & Stroke Center, MSC, Brooklyn, NY; 4University Hospital of Brooklyn, Associate Dean for Clinical Research & Faculty Development, Downstate Medical Center & Stroke Center
Corresponding Author: douglas.halket@downstate.edu
Journal MTM 6:3:7–13, 2017
doi:10.7309/jmtm.6.3.3
Background: Little is known about the prevalence and nature of mobile application adoption in clinical practice.
Aims: To explore current and potential mobile application use in primary care physicians (PCPs) for stroke prevention. Do PCPs recommend, use, or discuss mobile health applications for stroke preventative measures?
Methods: Current PCPs in the New York City area specializing in Internal Medicine, Ob/Gyn, and Family Medicine were surveyed in person. The survey consisted of demographic questions and 11 questions on mobile application use.
Results: Of the 86 physicians surveyed (53% female; mean age 37 years, SD 12), 74% (95% CI 65%, 84%) reported using mobile applications in patient care, whether for their own use or in recommending to patients. Experience was the most important determining factor, with 82% of physicians with less than 3 years practice experience using mobile apps, 78% of physicians with 3 to 10 years, 60% of physicians with 11 to 20 years, and 58% of physicians with greater than 20 years experience (p=0.045). Physicians reported using mobile applications to manage stroke risk factors 25% (95% CI 16%, 35%) of the time, while 77% (95% CI 68%, 86%) expressed interest in new apps to help their patients manage these risks. Lastly, 41% (95% CI 30%, 51%) of physicians surveyed strongly agreed that mobile applications are useful in providing patient care, while 49% (95% CI 38%, 59%) simply agreed and 0% disagreed.
Conclusions: Most urban PCPs we surveyed believe that mobile applications belong in healthcare, with one in four using them to manage stroke risk factors.
Keywords: Mobile Technology, Stroke, Prevention, Primary Care Physicians, Patient-Centered
Introduction
Stroke is the leading cause of preventable disability in the United States1. Each year, approximately 795,000 Americans suffer a stroke1. Many of these strokes are preventable. According to a case-control study of 6,000 individuals, 90% of strokes can be attributed to just 10 modifiable risk factors, and targeted interventions to reduce blood pressure and cigarette smoking as well as to promote physical activity and healthy diet could substantially reduce the risk of stroke2. There are already many mobile applications that individually target each one of these interventions, although not necessarily in the specific context of stroke prevention3.
Healthcare related mobile technology has expanded rapidly over the last several years. In 2015, there were 165,000 medical and health related apps for sale in the Google and Apple store4, up from 40,000 in 20125. However, little is known about the prevalence and nature of mobile application adoption in patient centered clinical practice, let alone about its effectiveness in changing healthcare outcomes. While there are many mobile applications in fields such as diabetes management, there are still usability and integration issues among almost all of them6. A 2014 study found 93 mobile application for iPhone and Android regarding general stroke information, although many of these were lacking scientifically valid information7.
There have been relatively few randomized controlled trials involving mobile applications, although some have shown promise. A systematic review of 9 studies assessing mobile application effectiveness in managing cardiovascular disease, lung disease, or diabetes mellitus found 3 studies where a mobile application intervention showed a statistically significant clinical improvement8. Additionally, there has been at least one quality improvement project studying mobile technology assistance in blood pressure control for stroke survivors9, although there have been no large scale randomized control trials specifically involving stroke prevention. Mobile applications have the potential to change the healthcare landscape, leading to improved outcomes while reducing cost. If mobile technology is going to be implemented in a meaningful way, it is imperative that it be grounded in clinical evidence.
The current study is the first step in examining the role that mobile technology plays in primary care physicians’ (PCPs’) practices. The purpose of this study is to examine the prevalence of PCPs using mobile applications in patient care. More specifically, to study if and how PCPs use mobile applications for stroke prevention. Also, we evaluated preferences and attitudes of PCPs toward the use of mobile applications in their practices with specific focus in stroke management, and how these preferences vary over physician and practice demographics. We hypothesize that younger physicians practicing in wealthier areas are more likely to use and recommend mobile applications.
Methods
Current PCPs in the New York City area specializing in Internal Medicine, Ob/Gyn, and Family Medicine were surveyed in person.
Participants: A convenience sample of 86 physicians (46 females) ranging from 25 to 68 years of age participated in this study, which was approved by the SUNY Downstate IRB. Participants were surveyed in person and were identified at SUNY Downstate grand rounds and the annual meeting of the New York Academy of Family Physicians. The mean age was 37 ± 12 SD. Forty one percent of the participants were attendings and the remaining 59% were residents. Sixty (70%) were Family Medicine specialists, 14 (16%) were in Ob/Gyn, and 12 (14%) were in Internal Medicine. These three specialties were selected because they provide the primary care lead in general preventative care, and the study focus is on actually managing stroke risk factors. Neurologists, despite managing patients after stroke, do not generally provide the ongoing lead in preventative care unless a patient has a separate neurological issue, and so were excluded from the study.
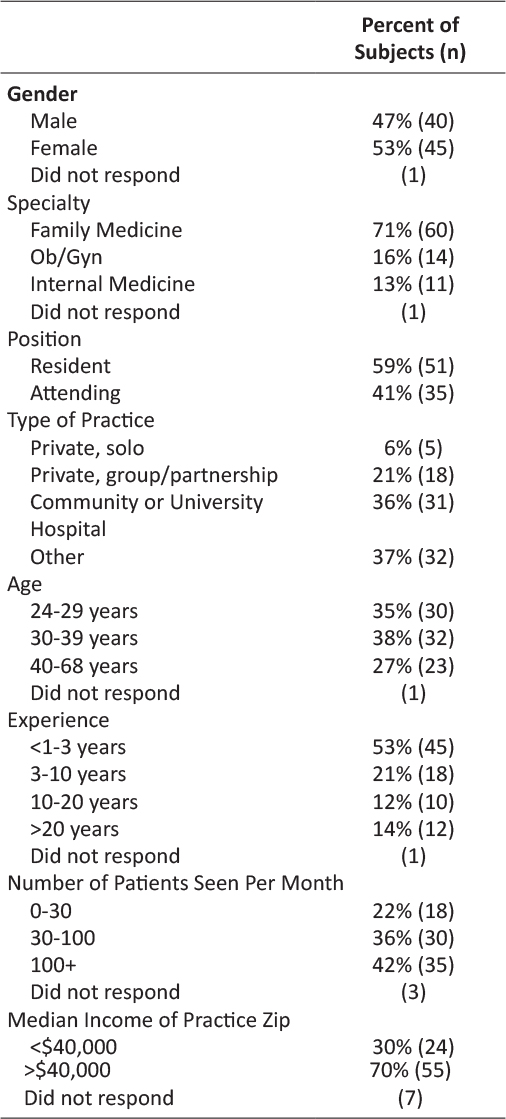
Measures: The standardized survey consisted of demographic questions and practice characteristics including gender, specialty, resident/attending, type of practice (private independent, private partnership, community or university hospital), years of experience (less than 3, 3 to 10, 11 to 20, greater than 20), patients seen per month (less than 30, 30 to 100, greater than 100), median income of practice zip code as determined by census data (less than $40,000 or greater than $40,000), and 11 questions on mobile application use (table 1).
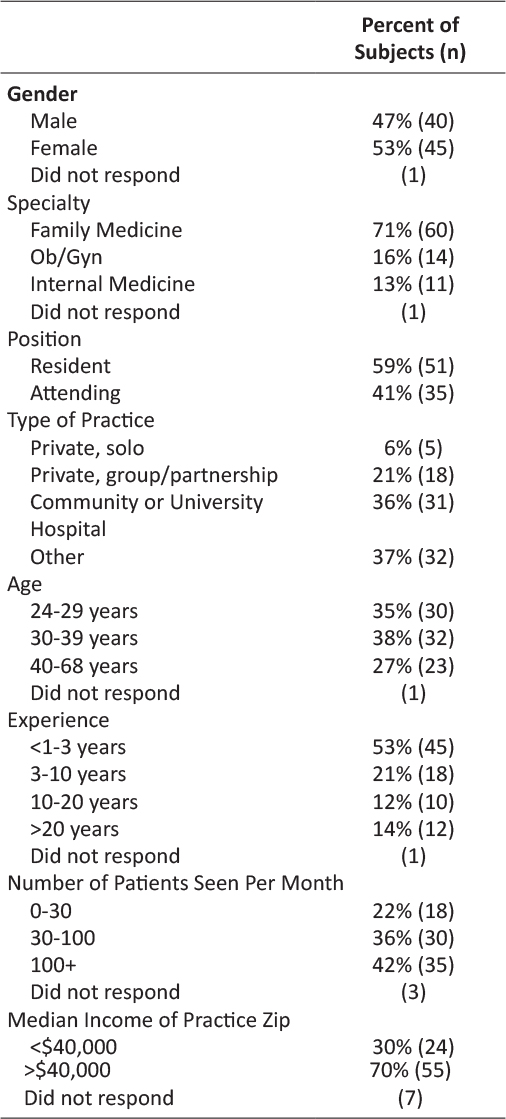
Table 1: Demographic Summary of Study Subjects
Data analysis: Fisher’s exact test was used to test for association between demographic variables and whether or not the physicians used mobile applications in any patient care setting. Cochran–Armitage trend test was used to determine if higher levels of the ordinal predictors (age groups, experience and volume of patients) were associated with higher prevalence of mobile technology use. P values less than 0.05 were considered significant. All participants answered the primary question on mobile application use in patient care. Missing data in other, secondary questions were not factored into the analysis as we were not adequately powered for other specific analyses. A sample size of 87 physicians was determined to have 80% power to detect an odds ratio of 0.4 for the relationship between age and the use of mobile applications using a significance level of 0.05. The odds ratio of 0.4 corresponds to a hypothesized effect of physician age on mobile application use. This odds ratio is based on an expected 30% use of mobile applications by physicians at age 50, compared to 15% for physicians at age 63. The data were analyzed using SAS version 9.4 (SAS Institute Inc., Cary, N.C.)
Results
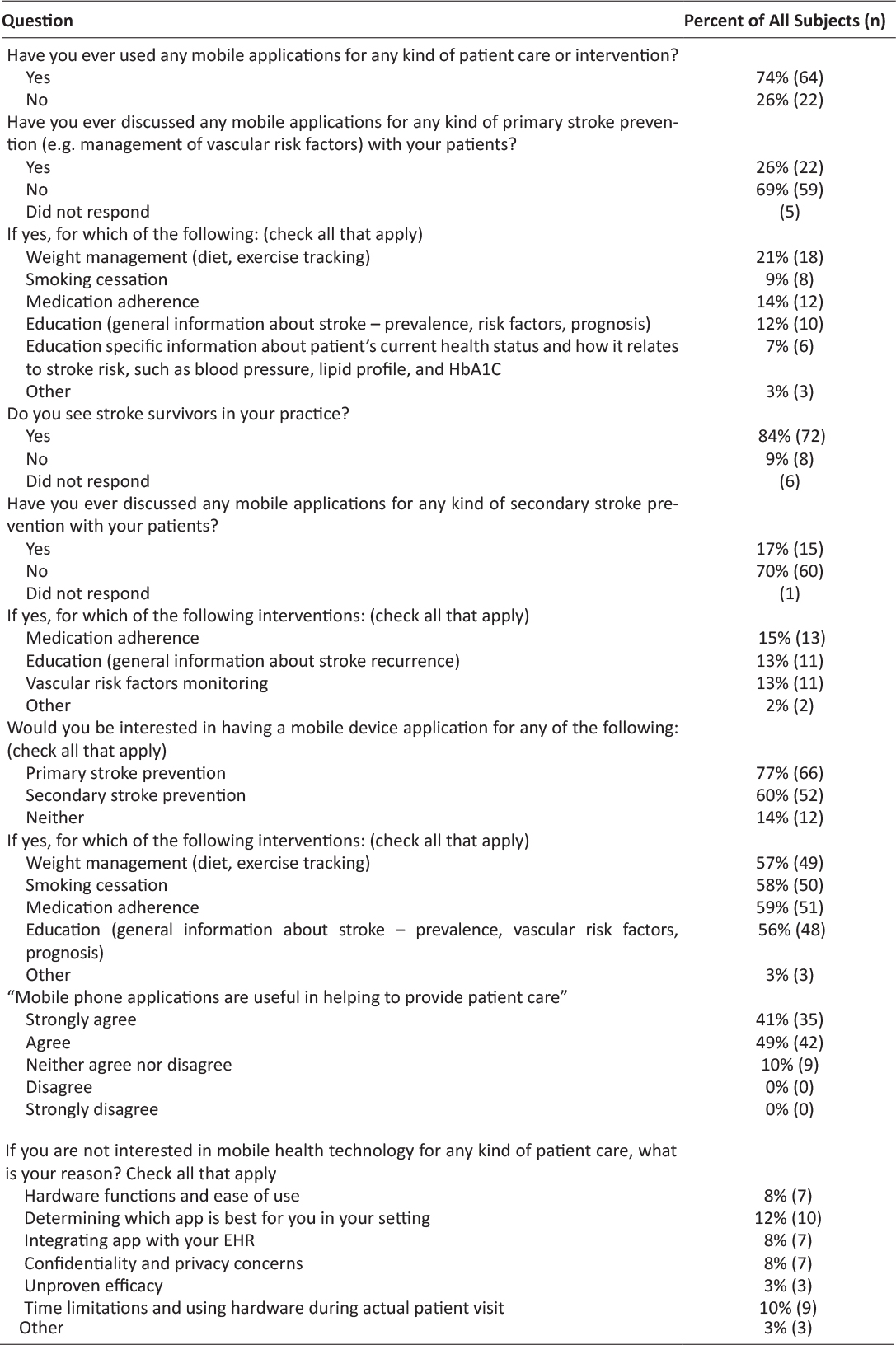
Of the 86 physicians surveyed, 74% reported using mobile applications in patient care, whether for their own use or in recommending to patients. Physicians reported using mobile applications to manage stroke risk factors 25% of the time, while 77% expressed interest in new apps to help their patients manage these risks. Forty one percent of physicians surveyed strongly agreed that mobile applications are useful in providing patient care, while 49% simply agreed and 0% disagreed.
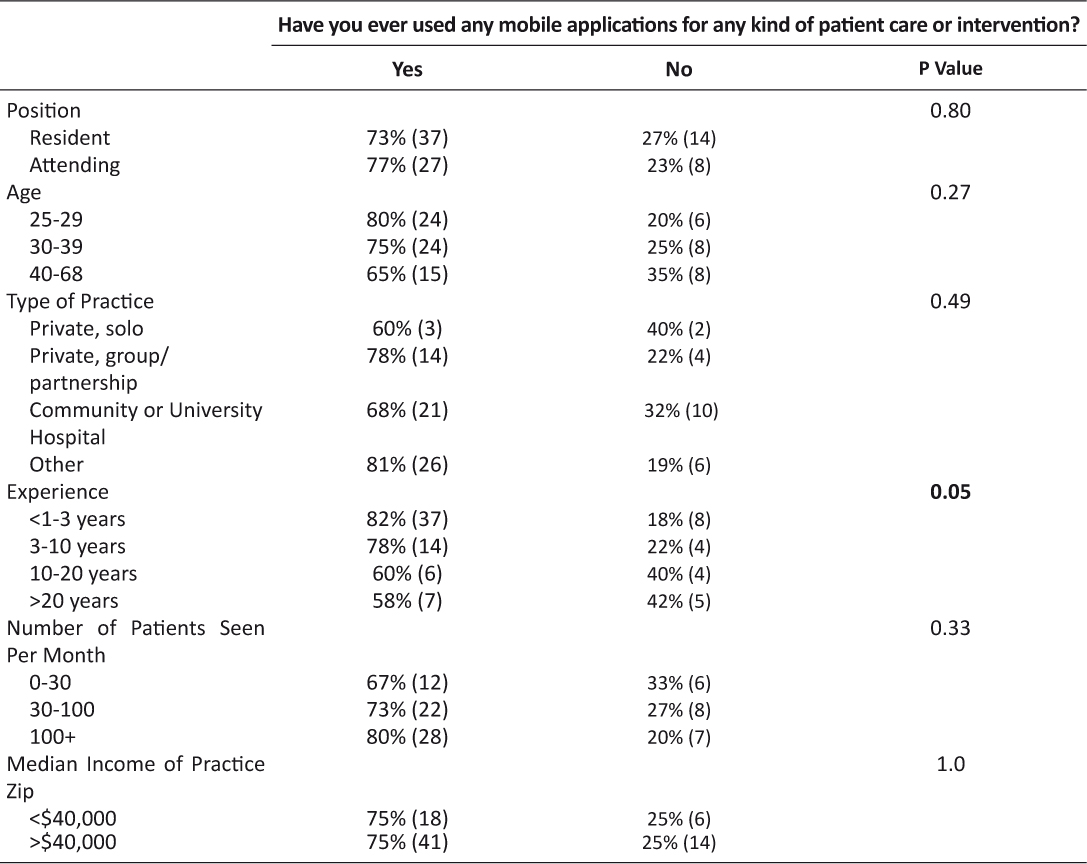
Table 2 shows the most important determining factor, with 82% of physicians with less than 3 years practice experience using mobile apps, 78% of physicians with 3 to 10 years, 60% of physicians with 11 to 20 years, and 58% of physicians with greater than 20 years experience (p=0.045). Other demographic factors, including median income of practice zip code were not significant.
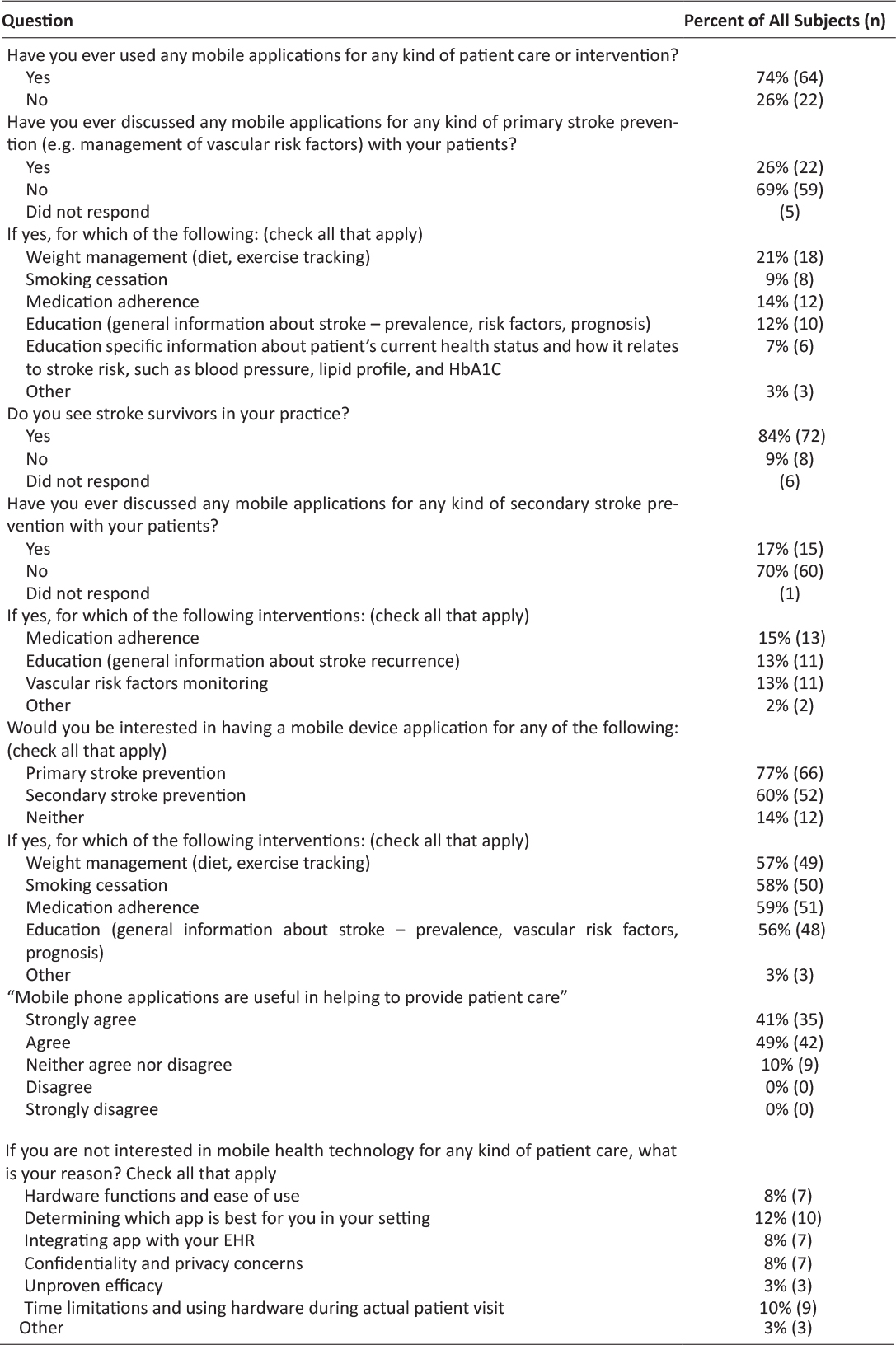
Table 2: Mobile Application Usage Responses
Age did not have an effect on whether or not physicians agree that mobile applications are useful in providing patient care (p=0.27; table 3). Position, type of practice, and volume of patients were not associated with higher use of mobile technology use (p=0.80, 0.49, 0.33, respectively).
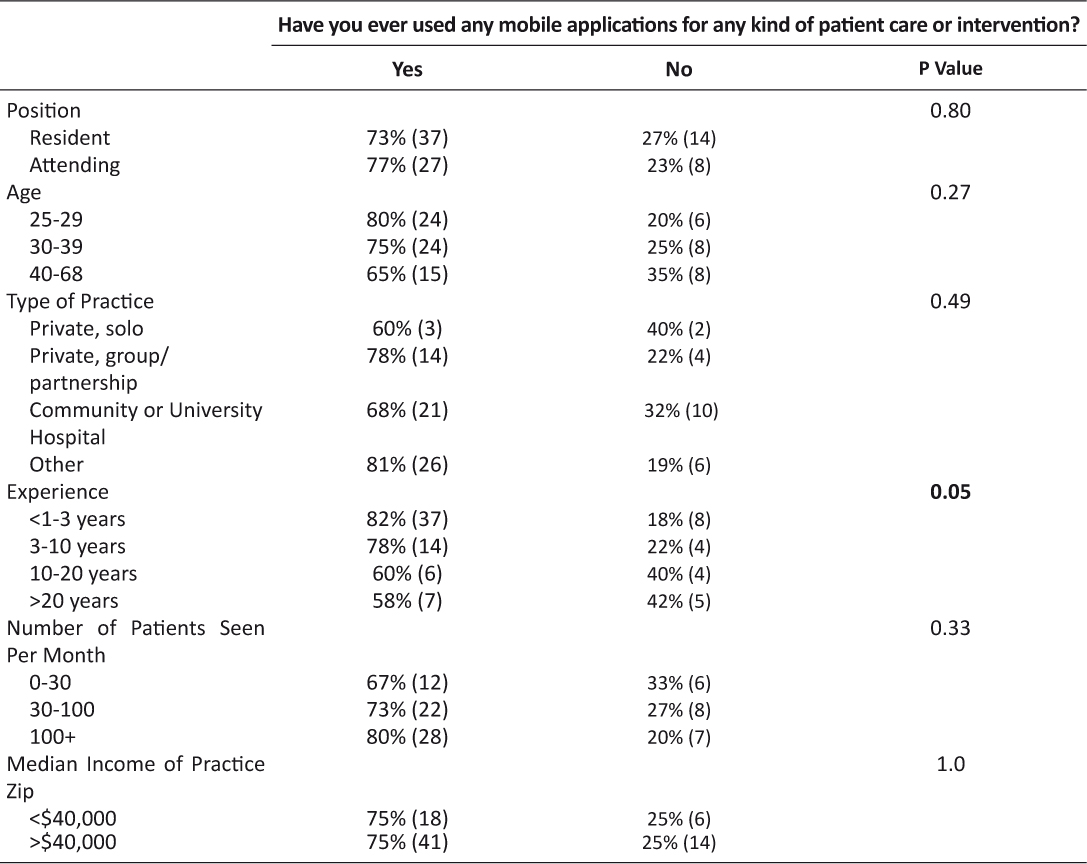
Table 3: Usage of Mobile Applications in Patient Care by Demographics
Discussion
Previous studies have shown that there are a large number of mobile applications available to patients and physicians, particularly to manage stroke risk factors3,4,6–8. This study builds on this knowledge in an attempt to determine how physicians view mobile application use in the primary care clinical setting, particularly in stroke prevention. Our data revealed that of a sampling of mostly urban PCPs, 74% are already using mobile applications in clinical practice and an even greater portion, 90%, believe that mobile applications belong in patient care. Although PCPs with more experience were less likely to use mobile applications, the findings suggest a wide acceptance across physician age groups and practice characteristics. Income of practice zip code was not a significant predictor in whether or not PCPs recommend mobile applications to patients, and neither was PCP age. Physician experience was potentially important, with less experienced PCPs more likely to recommend mobile applications than their more experienced colleagues. These findings suggest the adoption of mobile application use in clinical practice will likely continue to increase in the coming years.
Some physicians, 34% of the respondents, expressed concerns over mobile technology use in healthcare. These concerns included ease of use, confidentiality, determining which app is best, time limitations, and integration with Electric Health Records (EHR). Some of these concerns, such as determining which apps are best, can be solved with further study. Confidentiality and EHR integration issues are more complex but are also potentially manageable in the future5.
There was a major disparity between PCP-expressed interest in mobile applications (76%) compared with their actual use of mobile applications to manage stroke risk factors (25%). This gap between interest and use can be bridged by either the development of new mobile applications specifically tailored to manage stroke risk factors or the development of a tool to assist patients and physicians in selecting from already existing mobile applications. The development of such a tool would likely require a systematic method for determining which mobile applications are effective in the patient care setting. Mobile applications that can assist in managing chronic risk factors for stroke can then be identified, potentially leading to an inexpensive and effective method for reducing one of the largest causes of morbidity and mortality in the United States1,2.
There were several limitations to the study. First, the sample size was one under the projected number, as the data were collected from physicians in discrete groups (grand rounds, etc.) rather than from individuals. Second the data were slightly skewed by specialty and position. We recruited a large percentage of Family Medicine attendings because of the ease of recruiting them at their annual meeting. Many of the Ob/Gyn and Internal Medicine respondents were residents because they were more likely to attend grand rounds and stay to fill out a survey. There were few respondents from high income zip codes. We acknowledge the potential lack of generalizability to other specialties, including neurologists who may participate in stroke prevention but generally do not lead and primarily manage this effort in their patients.
Conclusions
The majority of PCPs have either already adopted mobile applications in their clinical practice or believe that mobile applications belong in patient care. However, the implementation of mobile applications specifically for stroke prevention purposes is still limited. Concerns about mobile application use were limited to a small number of physicians and a significant number expressed interest in a new application to manage stroke risk factors. There is PCP interest in a mobile application specifically tailored to manage stroke risk factors that patients and physicians can use together and encompasses several aspects of stroke prevention. Since many physicians are already using mobile applications or support their use in patient care, it is likely that mobile applications will have a place in clinical practice in the future, and specifically in stroke prevention.
Acknowledgements
Supported by a SUNY Alumni fund medical student research scholarship to DH.
Disclosures
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: DH received support from a SUNY Alumni grant, no other support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
References
1. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133(4):e38–360. 
2. O’Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet (London, England). 2010;376(9735):112–23. 
3. Mosa ASM, Yoo I, Sheets L. A Systematic Review of Healthcare Applications for Smartphones. BMC Medical Informatics and Decision Making. 2012;12:67. 
4. Misra S. New report finds that more than 165,000 mobile health apps now available, takes close look at characteristics & use: iMedicalApps; 2015 [updated September 17, 2015. Available from: http://www.imedicalapps.com/2015/09/ims-health-apps-report/.
5. West D. How mobile devices are transforming healthcare. Issues in technology innovation. 2012;18(1):1–11.
6. El-Gayar O, Timsina P, Nawar N, Eid W. Mobile Applications for Diabetes Self-Management: Status and Potential. Journal of Diabetes Science and Technology. 2013;7(1):247–62. 
7. Dubey D, Amritphale A, Sawhney A, Amritphale N, Dubey P, Pandey A. Smart phone applications as a source of information on stroke. Journal of stroke. 2014;16(2):86–90. 
8. Whitehead L, Seaton P. The Effectiveness of Self-Management Mobile Phone and Tablet Apps in Long-term Condition Management: A Systematic Review. Journal of medical Internet research. 2016;18(5):e97. 
9. Ovbiagele B, Jenkins C, Patel S, Brunner-Jackson B, Anderson A, Saulson R, et al. Mobile health medication adherence and blood pressure control in recent stroke patients. Journal of the neurological sciences. 2015;358(1–2):535–7. 
Read More