Clinical Application of a Smartphone-Based Ophthalmic Camera Adapter in Under-Resourced Settings in Nepal
Clinical Application of a Smartphone-Based Ophthalmic Camera Adapter in Under-Resourced Settings in Nepal
Carmel Mercado, MD1, John Welling, MD2,3,4, Matthew Oliva, MD3,4,5, Jack Li, MD2, Reeta Gurung, MD6, Sanduk Ruit, MD6, Geoff Tabin, MD1,3,8, David Chang, MD7, Suman Thapa, MD, PhD6, David Myung, MD, PhD1,8
1Byers Eye Institute, Stanford University, Palo Alto, CA, USA; 2John A Moran Eye Center, University of Utah, Salt Lake City, Utah, USA; 3Himalayan Cataract Project, Waterbury, VT, USA; 4Medical Eye Center, Medford, OR, USA; 5Casey Eye Institute, Oregon Health Sciences University, Portland, OR, USA; 6Tilganga Institute of Ophthalmology, Kathmandu, Nepal; 7Los Altos Eye Physicians, Los Altos, CA, USA; 8VA Palo Alto Health Care System, Palo Alto, CA, USA
Correspondence Author: david.myung@stanford.edu
Journal MTM 6:3:34–42, 2017
Background: The ability to obtain high quality ocular images utilizing smartphone technology is of special interest in under-resourced parts of the world where traditional ocular imaging devices are cost-prohibitive, difficult to transport, and require a trained technician for operation.
Purpose: The purpose of this study was to explore potential anterior and posterior segment ocular imaging use cases for a smartphone-based ophthalmic camera adapter (Paxos Scope, Digisight Technologies, San Francisco, CA, USA) in under-resourced settings in Nepal.
Methods: From September to November of 2015 we utilized the Paxos Scope smartphone camera adapter coupled with an iPhone 5 to explore anterior and posterior segment clinical applications for this mobile technology. We used the device at a tertiary eye care facility, a rural eye hospital and a rural cataract outreach camp. We tested the device’s capability for high quality photo-documentation in clinic, in the operating room, and in the outreach camp setting. Images were automatically uploaded to a secure, cloud-based electronic medical record system that facilitated sharing of images with other providers for telemedicine purposes.
Results: Herein we present 17 ocular images documenting a wide variety of anterior and posterior segment pathology using the Paxos Scope from clinical cases seen in a variety of settings in Nepal.
Conclusions: We found the quality of both the anterior and posterior segment images to be excellent in the clinic, the operating room, and the outreach camp settings. We found the device to be versatile and user-friendly, with a short learning curve. The Paxos Scope smartphone camera adapter may provide an affordable, high-quality, mobile ocular imaging option for under-resourced parts of the world.
Keywords: Paxos Scope, mobile health, smartphone ophthalmic imaging, teleophthalmology, triage
Introduction
Worldwide there are an estimated 285 million people suffering from vision impairment and 39 million who are blind. ‘Low vision’ is defined as visual acuity of less than 6/18 but equal to or better than 3/60 or a corresponding visual field loss to less than 20 degrees in the better eye; ‘blindness’ is defined as visual acuity of less than 3/60 or a corresponding visual field loss to less than 10 degrees in the better eye; and ‘visual impairment’ includes both low vision and blindness.1 The World Health Organization predicts that 80% of these are preventable cases, and 90% of these individuals are located in low-income countries where access to eye care is limited. As life expectancy and standard of living have improved in many parts of the world, the burden of blinding eye disease has increased with the aging population. In the last decade, other than cataracts, glaucoma, corneal opacities, age related macular degeneration and diabetic retinopathy have emerged as some of the most common causes of preventable blindness.2,3 As blindness can be avoided in all of these conditions if diagnosed and treated early there is an urgent need to expand screening capabilities for these conditions. However, such screening can be challenging in resource-limited settings for a variety of reasons such as lack of health infrastructure, lack of trained eye health personnel, and the inability to obtain cost prohibitive ophthalmic equipment.
Eye health personnel have been using imaging equipment such as ophthalmoscopes since the 1800s.4 Anterior and posterior segment imaging have since become an integral part of an eye clinic, aiding in the diagnosis and monitoring of eye diseases. Advancements in digital imaging have continued to improve the way we are able to capture, process, and share images.5 Moreover, the advent of mobile technology coupled with digital imaging has paved the way for telemedicine to address public health issues.6
There are an estimated 6.8 billion mobile phone subscriptions across the world, and nearly 40% of the world’s population is online.7 Mobile health, defined as the use of mobile devices in patient care and public health, has experienced an increase in popularity over recent years.8 One area of innovation which has garnered significant interest is the ability to obtain, share, and analyze high quality ocular images utilizing mobile camera technology. This capability holds special interest in under-resourced parts of the world where traditional ocular imaging devices are difficult to transport, cost-prohibitive and require a trained technician for operation9,10.
Mobile ophthalmic imaging devices have shown promise in revolutionizing ophthalmic care. In 2014, Myung et al. reported on a prototype adapter for external eye and fundus imaging, with the latter being a 3D printed adapter that mounts a condensing lens to a smartphone to turn it into an indirect ophthalmoscope.11 Toy et al. compared images taken with a subsequent iteration of this device with in-person slit-lamp biomicroscopy for grading diabetic retinopathy and found 90% agreement between the two methods; moreover, they found that the photograph grade was 91% sensitive and 99% specific, with a 95% positive predictive value and a 98% negative predictive value, for diabetic disease in their patient population.12 These devices were the early prototypes of a now-commercially available device known as Paxos Scope™ (DigiSight Technologies, San Francisco, CA, USA) that was registered in 2015 with the United States Food and Drug Administration (FDA) as a 510(k) Class II exempt ophthalmic camera for both anterior and posterior segment photography. In parallel efforts, Maamari et al. (2014) described a digital fundus imaging device for taking high quality wide field retinal photographs,13 while Russo et al. (2015) published a study using a direct ophthalmoscopy adapter (D-Eye) for diabetic screening, which also showed excellent agreement between in-person and smartphone image-based retinopathy grading. Russo’s group found exact agreement between the two methods of retinopathy grading in 204 of 240 eyes (85%) and agreement within 1 grade level of diabetic retinopathy in 232 of 240 eyes (96.7%).14 Teleophthalmology has been shown to be an effective tool for diagnosing diabetic retinopathy and macular edema15 well before the advent of high resolution smartphone cameras, and these above studies suggest an emerging role for smartphones for this purpose. In addition, Kanagasingam et al. (1999) and Bastawrous et al. (2016) evaluated the potential for teleophthalmologic diagnosis and screening of glaucoma using a portable fundus camera and smartphone-based retinal adapter, respectively, and found the camera and smartphone adapter provided similar reliable diagnostic results.16,17 Thus, there is a growing consensus about the potential for smartphone-based imaging to enhance teleophthalmology.
In this paper, we test the utility of Paxos Scope system at the Tilganga Institute of Ophthalmology (TIO) in Kathmandu, Nepal and at TIO’s rural outreach centers. Eighty-three percent of Nepalese live in rural settings18 with very limited access to an ophthalmologist as there are only 217 ophthalmologists and ophthalmologists-in-training in the country, most of whom are located in metropolitan areas.19 Two of the authors (JW and MO) spent significant time at TIO and its outlying rural community eye centers (CECs), using the device in various clinical settings where ophthalmic photography was otherwise unavailable. We present our experience using this device in Nepal and its potential applications in the developing world. In our experience, the Paxos Scope’s portability, ease of use, and low cost make this technology especially applicable to the developing world.
Methods
JW and MO are both cornea specialists who visited Nepal as part of the Himalayan Cataract Project from September to November 2015. They spent time at TIO, the Geta Eye Hospital, a rural hospital in Danghadi, Nepal, and the rural outreach cataract camps in Hetauda, Nepal during this trip (Figure 1). They obtained photographs using the Paxos Scope in all of these settings as part of documentation for the patients’ records. Patient consent was obtained prior to acquisition of all photographs.

Figure 1: Example of the rural settings in which the
Paxos Scope was used for imaging documentation
The smartphone-based imaging system consisted of an iPhone 5 (Apple Inc, Cupertino, CA, USA) camera phone (8 megapixel resolution) and the Paxos Scope anterior and posterior segment hardware adapters with external light-emitting diode (LED) illumination (Figure 2; Stanford University, Palo Alto, CA, USA, described in detail previously11,20). To obtain anterior segment photographs, the adapter consisting of a macro lens and external LED was attached to the phone. The LED light on the adapter was first turned on. No other illumination settings were required beyond turning the external light source on. The patient was then instructed to fixate on a target straight ahead with eyes wide open. The phone, held in landscape orientation, was then brought straight-on to within approximately 5 centimeters of the patient’s orbital rim until iris details, such as the pupillary margin, were in focus. To obtain fundus photographs, a Volk 20D lens (Volk Optical, Inc, Mentor, OH, USA) mounted onto the posterior segment adapter was first attached to the phone. The adapter consisted of a 14.6 centimeter (5.75 inch) long lens-to-smartphone mount with a sliding shaft that could be lengthened to allow adjustment of the working distance between the phone and the lens. The external LED of the Paxos unit is used as the source of illumination. The patient was instructed to fixate on a target straight ahead, then the phone-adapter complex was stabilized with fingers braced on the patient’s brow and cheek in similar fashion to the hand position for indirect ophthalmoscopy. The axis formed by the indirect lens and camera was initially directed nasally toward the optic nerve. Once the optic nerve was in focus, the view was then tilted temporally so the macula could also be captured in the photograph.

Figure 2: Photograph of Paxos Scope anterior and posterior segment hardware adapters with external light-emitting diode illumination attached to an iPhone (Apple Inc, Cupertino, CA, USA)
In settings where wi-fi was available, participant photographs were uploaded to a secure, HIPAA-compliant, cloud-based server (www.digisight.net) and later paired with the patient’s electronic medical record at the respective clinic sites. All image acquisition and transmittal was handled with strict attention to the confidentiality of personal data in accordance with the Data Protection Act of 1998 and Access to Health Records of 1990.
Results
Herein we include a series of ocular photographs taken with the Paxos Scope while in Nepal. All photographs included in this section were obtained by the first author, JW, who had less than 2 months experience with the Paxos Scope prior to utilization and no prior formal training with the device.
Figures 3–7 were taken within the TIO Outpatient Department in Kathmandu, Nepal, the main eye center in Nepal. First built in the early 1990s through the combined efforts of the Nepal Eye Program, the Himalayan Cataract Project, the Fred Hollows Foundation, Tissue Banks International in Baltimore, USA, and Lions International, this tertiary eye care facility remains today the flagship institution for the Himalayan Cataract Project. TIO is the main central training center for ophthalmologists for the entire country, with all ophthalmologic subspecialties represented. These images represent a small sample of the myriad pathology commonly seen at TIO.
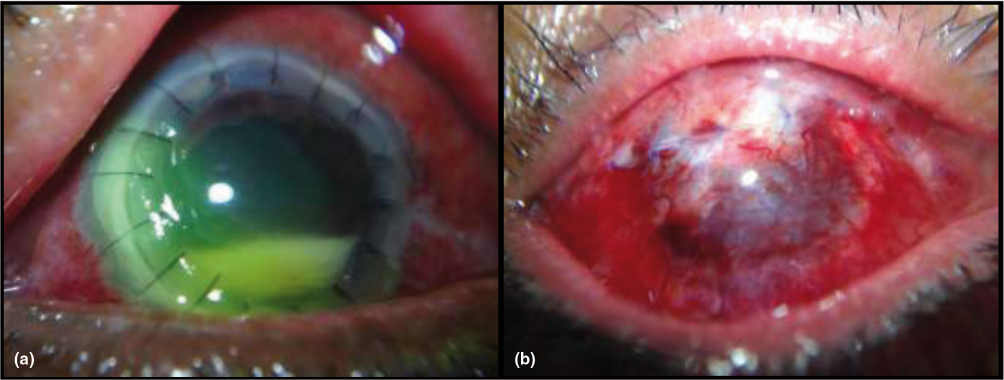
Figure 3 a-b: Anterior segment photos obtained in the clinic documenting (a) the recurrence of a fungal ulcer after penetrating keratoplasty and (b) post-operative day 1 appearance following conjunctival flap in the same eye
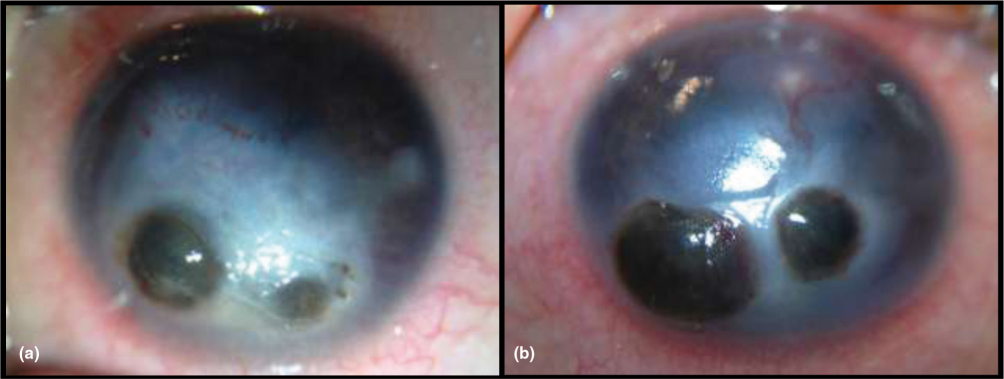
Figure 4 a-b: Anterior segment images of the (a) right and (b) left eye obtained intra-operatively showing bilateral corneal perforations due to vitamin A deficiency in a malnourished 7 year old female. The patient subsequently underwent penetrating keratoplasty of the left eye
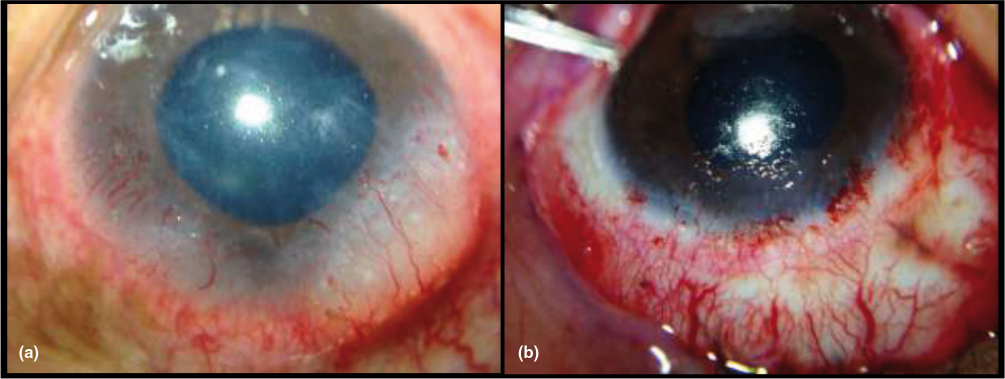
Figure 5 a-b: Intra-operative anterior segment photos showing a limbal lesion that extends from the 3 o’clock to 9 o’clock position (a) prior to excision and (b) immediately following excisional biopsy
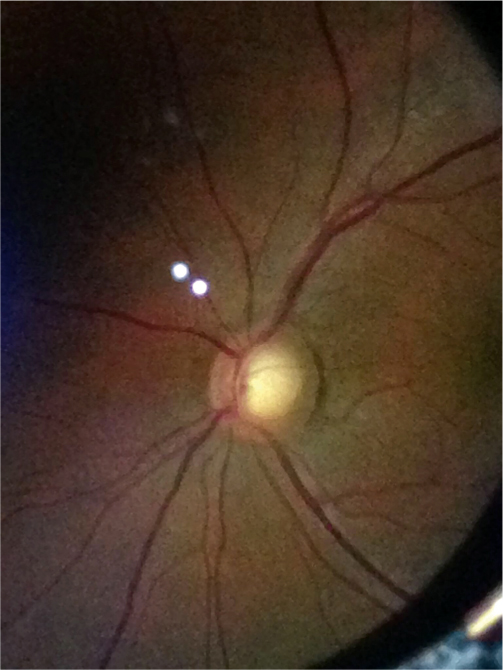
Figure 6: Posterior segment image obtained in clinic within the first week of visit to document optic nerve appearance (left eye) in a glaucoma suspect
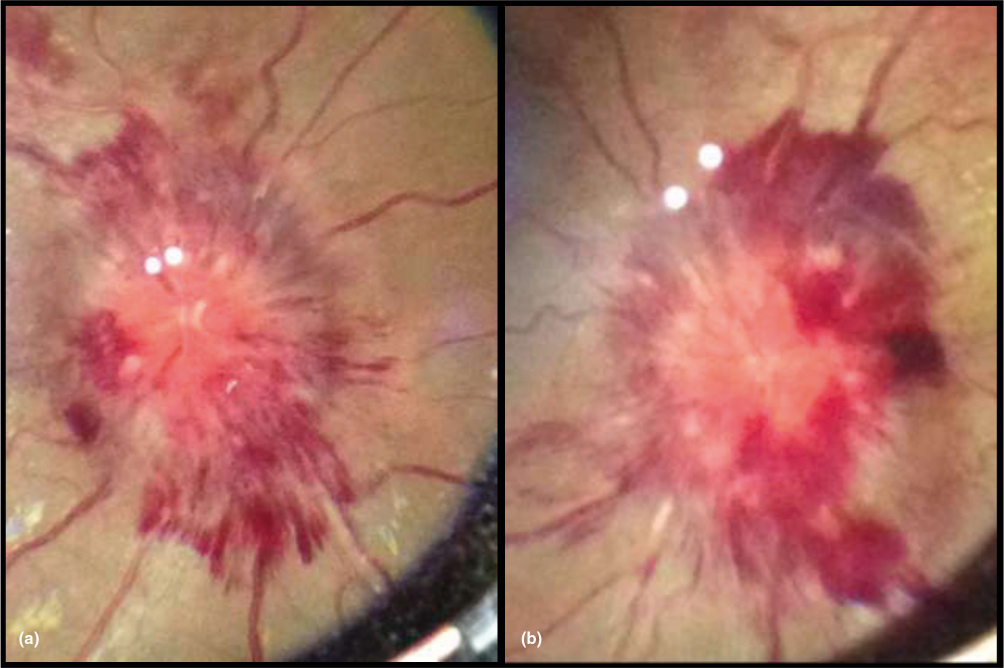
Figure 7 a-b: Posterior segment images obtained in clinic showing severe bilateral optic nerve edema and peripapillary hemorrhage in a patient found to have tuberculous meningitis. Right eye (a) and left eye (b) are shown
Figures 8–11 were taken in two remote eye care facilities in Nepal (Geta Eye Hospital, Dhangadhi, Nepal [Figures 8–10] and Hetauda, Nepal [Figure 11]). Geta Eye Hospital is a rural eye hospital in the far western portion of Nepal known as Biratnagar. Geta Eye Hospital is centrally located in the forest of Geta village near the Indian border and provide care to both the Nepalese and Indian populations. Yearly it is estimated that more than 40,000 cataract surgeries are performed here. Ophthalmologists also have the option of telemedicine consultation with TIO for management of complex cases. The Hetauda Community Eye Hospital, similar to the Geta Eye Hospital, was established in 2007 to help the rural communities south of Katmandu. Health care workers and residents from TIO rotate through Hetauda for training after residency.
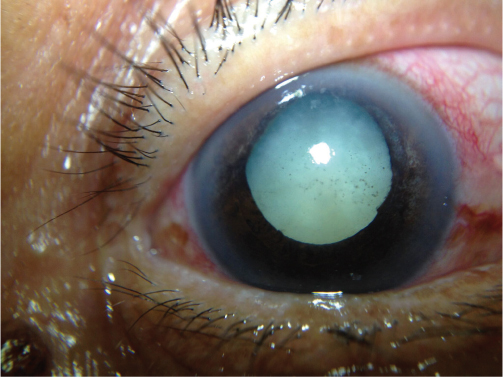
Figure 8: Anterior segment image obtained in the clinic to document phacomorphic angle closure glaucoma
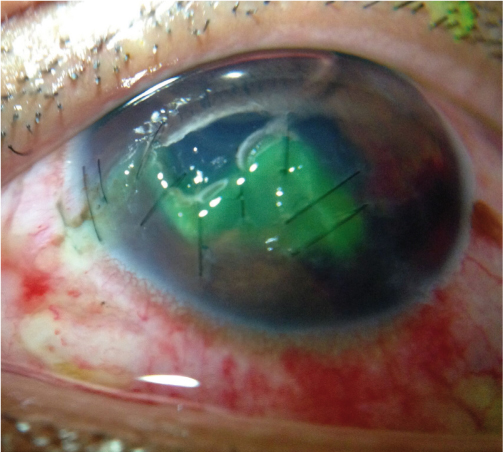
Figure 9: Anterior segment image obtained in clinic to document the appearance of a complex corneal laceration repair on post-operative day 1 (right eye, following instillation of fluorescein dye). Agriculture-related eye trauma are common in these communities
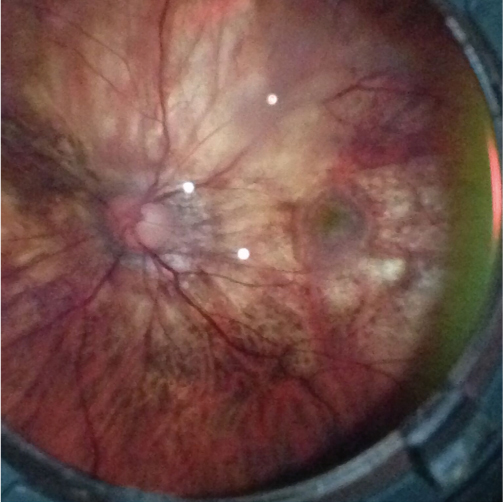
Figure 10: Posterior segment image showing myopic degeneration with sub-foveal choroidal neovascularization in a left eye

Figure 11: Posterior segment image of a left eye with a toxoplasmosis lesion in the inferior retina with characteristic overlying vitritis
Figures 12–13 were obtained at a cataract outreach camp in Hetauda, Nepal. These images are representative of the pre-operative and post-operative cataract surgery photos taken at the camp.
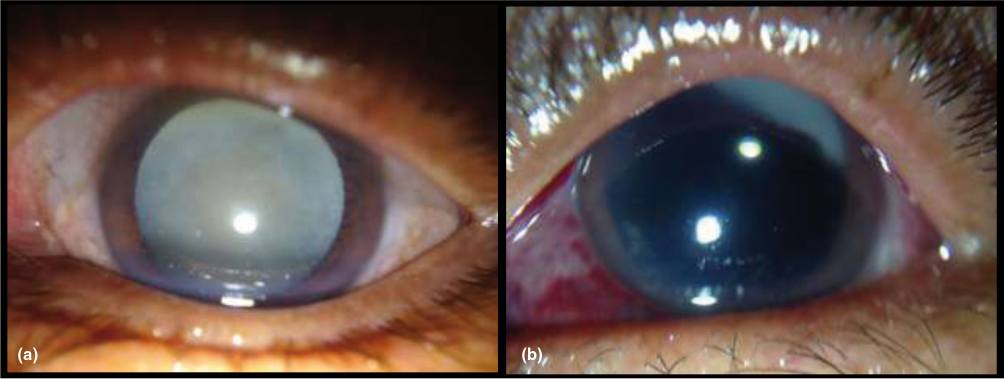
Figures 12 a-b: Anterior segment images showing (A) pre-operative appearance of a mature cataract and (B) post-operative day 1 appearance following manual small incision cataract surgery with posterior chamber intraocular lens implantation in the same eye
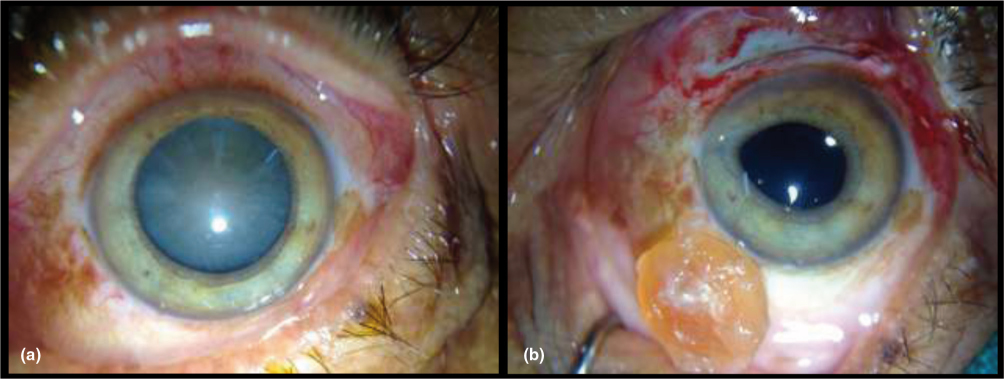
Figure 13 a-b: Anterior segment images taken intra-operatively showing the appearance of a mature cataract (A) before and (B) after extraction via manual small incision cataract surgery with posterior chamber intraocular lens implantation
Discussion
We demonstrate the use of the Paxos Scope smartphone camera adapter in a variety of settings, not only in the clinic but within the surgical field as well as in outreach camps. In our experience the Paxos Scope is a powerful and high-quality ophthalmic imaging device of the front and back of the eye. It is easily portable, low maintenance, and harnesses the capabilities of smartphones which are already ubiquitous. It has previously been shown that patients are comfortable throughout imaging when being photographed with this system and have high tolerance to the LED light attached to the adapter.21 Furthermore, image acquisition added only an additional 2-5 minutes on average to the exam based on the authors’ experiences. During our visit, we began to incorporate principles of telemedicine using the Paxos Scope images as a way to relay information between the rural hospital setting and TIO, The Paxos Scope was also helpful as a teaching tool. By obtaining images in real time, we were able to share clinical findings with the residents and fellows and begin to create a database for case studies and presentations. The images were also helpful in patient education.
There are some limitations noted with the use of the Paxos Scope. Notably, the Paxos Scope was best used in dark settings. If used outdoors or in well-lit areas such as in the outreach camps, the fundus photos were more difficult to obtain. Patients also needed to be well-dilated to take the fundus images as the Paxos Scope is not a non-mydriatic camera. Another limitation was with the use of the Digisight software. Many areas we visited in Nepal did not have good wi-fi and some of the applications of telemedicine were thus limited by our connectivity. Initially we also did not have the capabilities to take photos while offline, but with updates in the software midway through our trip, we were later able to upload images from the photo gallery on our phones, thus by-passing this issue. There was also a learning curve to taking images with the adapter but this was relatively short and did not require special training. Author JW was able to learn the Paxos Scope system within the first ten imaging acquisition attempts, which agrees in time course with Ludwig et al.’s previous study on the ease of use of the Paxos Scope.21
In rural underserved countries like Nepal, this device has the capacity and potential to expand telemedicine by (1) empowering community eye hospitals to relay information back and forth with tertiary eye centers like TIO and (2) providing a means through which subspecialty trained physicians concentrated in the cities could extend their impact and influence to help in rural areas. This pilot experience sets the stage for a study that is forthcoming, where we are looking at training CEC-based ophthalmic technicians to use the Paxos Scope for both anterior and posterior segment imaging and send these images for triage and treatment to trained physicians at TIO. We anticipate through this future study we will be able to establish a model of remote triaging and management which could be applicable to under-resourced settings in other countries.
Conclusion
The Paxos Scope smartphone camera adapter’s portability, ease of use, and low cost may provide an affordable, high-quality, mobile ocular imaging option for under-resourced parts of the world.
Acknowledgements
The authors would like to thank the American Society of Cataract and Refraction Surgeons (ASCRS) Foundation for its generous donation to the Himalayan Cataract Foundation to help with the acquisition of Paxos Scope adapters, and the Himalayan Cataract Foundation for their support of authors JW and MO. The Byers Eye Institute at Stanford acknowledges support from the Research to Prevent Blindness Foundation.
Disclosure: Author DM is a co-inventor on a patent for the Paxos Scope device and is a consultant to DigiSight Technologies.
References
1. World Health Organization. International statistical classification of diseases, injuries and causes of death, tenth revision. Geneva, 1993.
2. Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol 2012;96:614–8. ![]()
3. Bastawrous A, Hennig BD. The global inverse care law: a distorted map of blindness s. Br J Ophthalmol. 2012;96(10):1357-1358. ![]()
4. Sherman SE.The history of the ophthalmoscope. Doc Ophthalmol. 1989;71(2):221- 228. ![]()
5. Hildred RB. A brief history on the development of ophthalmic retinal photography into digital imaging. J Audiov Media Med. 1990;13(3):101-105. ![]()
6. Tachakra S, Wang XH, Istepanian RS, Song YH. Mobile e-health: the unwired evolution of telemedicine. Telemed J E Health. 2003;9(3):247- 257. ![]()
7. Tarczy-Hornoch K, Cotter SA, Borchert M, et al. Prevalence and causes of visual impairment in Asian and non-Hispanic white pre- school children: Multi-ethnic Pediatric Eye Disease Study. Ophthalmology. 2013;120(6):1220-1226. ![]()
8. Ludwig C, Callaway N, Park JH, Leng T. Mobile Health in the Retinal Clinic Population: Access to and Interest in Self-Tracking. Ophthalmic Surgery, Lasers & Imaging Retina. 2016; 47:252-257. ![]()
9. Breslauer DN, Maamari RN, Switz NA, Lam WA, Fletcher DA. Mobile phone based clinical microscopy for global health applications. PLoS One. 2009;4(7):e6320 ![]()
10. Chakrabarti R. Application of mobile technology in ophthalmology to meet the demands of low-resource settings. J Mob Technol Med 2012;1:1–4. ![]()
11. Myung D, Jais A, He L, et al. 3D Printed Smartphone Indirect Lens Adapter for Rapid, High Quality Retinal Imaging. J Mob Technol Med 2014;3:9–15. ![]()
12. Toy B, Myung D, He L, Pan CK, Chang RT, Polkinhorne A, Merrell D, Foster D, Blumenkranz M. Smartphone-Based dilated fundus photography and near visual acuity testing as inexpensive screening tools to detect referral warranted diabetic eye disease. Retina 36:1000–1008. ![]()
13. Maamari RN, Keenan JD, Fletcher DA, et al. A mobile phone-based retinal camera for portable wide field imaging. Br J Ophthalmol 2014;98:438–41. ![]()
14. Russo A, Morescalchi F, Costagliola C, et al. Comparison of smartphone ophthalmoscopy with slit-lamp biomicroscopy for grading diabetic retinopathy. Am J Ophthalmol 2015;159:360–4.e1. ![]()
15. Whited JD. Accuracy and Reliability of Teleophthalmology for diagnosing Diabetic Retinopathy and Macular Edema: A Review of the Literature. Diabetes Technol Ther 2006;8. ![]()
16. Kanagasingam, Yogesan, PHD, Constable, Ian J., FRACO, Barry, Chris J., MMedSc, Eikelboom, Robert H., PHD, Morgan, William, FRACO, Tay-Kearney, Mei-ling, FRACO, Jitskaia, Ludmila M. Evaluation of a Portable Fundus Camera for Use in the Teleophthalmologic Diagnosis of Glaucoma. J. Glaucoma. 1999;8:297–301.
17. Bastawrous A, Giardini ME, Bolster NM, Peto T, Shah N, Livingstone IA, Weiss HA, Hu S, Rono H, Kuper H, Burton M. Clinical Validation of a Smartphone-Based Adapter for Optic Disc Imaging in Kenya. JAMA Ophthalmol. 2016 Feb;134(2):151-8. ![]()
18. Central Bureau of Statistics. Nepal Multiple Indicator Cluster Survey 2014, Key Findings. Kathmandu, Nepal: Central Bureau of Statistics and UNICEF Nepal.
19. International Council of Ophthalmology. Nepal Ophthalmic Society Directory 2016. Kathmandu, Nepal.
20. Myung D, Jais A, He L, Chang RT. Simple, low-cost smart- phone adapter for rapid, high quality ocular anterior segment imaging: a photo diary. J Mob Technol Med 2014;3:2–8. ![]()
21. Ludwig CA, Murthy SI, Pappuru RR, Jais A, Myung D, Chang RT. A novel smartphone ophthalmic imaging adapter: User feasibility studies in Hyderabad, India. Indian Journal of Ophthalmology, 2016, Vol 64, Issue 3:191-200.

