A Pilot Study of Using a Personalised Video Message Delivered by Text Message to Increase Maternal Influenza Vaccine Uptake
Khai Lin Kong, MBBS1, Sushena Krishnaswamy, MBBS, PhD1, Ryan Begley, MD, BSc2, Paul Paddle, MBBS2,3,4, Michelle L. Giles, MBBS, PhD1
1Department of Obstetrics and Gynaecology, Monash University, Melbourne, Australia
2Nebula Health, Melbourne, Australia
3Department of Otolaryngology, Head & Neck Surgery, Monash Health, Melbourne, Australia
4Department of Surgery, Monash University, Melbourne, Australia
Corresponding Author: Sushena.krishnaswamy@monashhealth.org
Background: Despite influenza vaccination being recommended, widely accessible and available free of charge for all pregnant women in Australia, vaccine coverage remains low. Novel strategies to increase uptake of influenza vaccine by pregnant women need to be explored.
Aims: This report aims to describe the implementation of a customised educational video about maternal influenza vaccination sent by text message, and its impact on maternal influenza vaccine uptake.
Methods: We trialled a customised video message as a strategy to improve maternal influenza vaccination coverage. Two hospitals in regional Victoria produced videos featuring senior local maternity care providers conveying information on the seriousness of maternal influenza infection and the benefits of maternal influenza vaccine. A link to the video was sent via text message to all pregnant women registered to give birth at that health service. Women were subsequently asked to complete a questionnaire about access to and relevance of the video.
Results: In May and August 2019 respectively, 842 and 742 text messages were sent. 233 pregnant women completed the questionnaire. 72 (31%) recalled receiving a text message. 26/72 (36%) of respondents watched the video, and 35% were motivated to receive influenza vaccine by the video. More than 70% of those who viewed the video confirmed that it was relevant and easy to understand.
Conclusion: Sending health information using a personalised video delivered via text message is a novel and acceptable method to provide maternal vaccine recommendation to pregnant women. This intervention could be considered along with other strategies to improve maternal vaccine uptake.
Keywords: maternal immunisation, text message video link, health promotion, influenza vaccine, pregnancy
Introduction
Influenza disease causes significant morbidity and mortality for pregnant women and may lead to adverse fetal and neonatal outcomes.1,2 Influenza vaccine has been demonstrated to protect pregnant women from severe influenza infection.3,4 The protective effect of vaccinating pregnant women (maternal immunisation) extends to their infants and has been demonstrated to reduce the incidence of influenza infection in the first six months of life.5 Despite the evidence of benefit of maternal influenza vaccination, access to the vaccines free of charge, and national recommendation for pregnant women to receive influenza vaccine in Australia, vaccine uptake remains low, with reported uptake ranging from 25to 61%.6–9
Healthcare provider recommendation of a vaccine during pregnancy is one of the most important factors associated with a woman’s decision to be vaccinated.10,11 While traditionally healthcare provider recommendation has been delivered from provider to patient during a consultation, new technologies such as text messages, links to credible websites etc. can be utilised to augment health promotion messaging. In terms of maternal immunisation, automated text messages with information about maternal influenza vaccine have been trialled in two randomised controlled trials.12,13 One study included information about influenza vaccine along with routine text message appointment reminders. This study reported a 30% increase in vaccine uptake compared to those who only received appointment reminders.12 Another study compared use of text messages conveying general health information related to pregnancy with and without influenza vaccine information. No difference in vaccine uptake was noted between the two groups.13 Two randomised controlled trials have examined using videos with recommendations on maternal vaccines as a strategy to improve uptake.14,15 Pregnant women allocated to the video intervention arm were given time at their antenatal clinic appointment to watch the video on a handheld device provided by the investigators. Neither of these studies reported a significant impact on maternal vaccine uptake, and neither of these studies examined sending the video directly to the pregnant woman’s personal device.14,15
A systematic review identified 28 studies that used mobile phone technology as an intervention to improve a variety of maternal-fetal health outcomes, in areas such as smoking cessation and weight management.16 While the outcomes were mixed in this review, it concluded that using mobile phone technology such as text messaging could be utilised to deliver health messages to pregnant women.
In this study, we assess an innovative approach of delivering a customised video featuring local maternity care providers, directly to the woman’s mobile phone via text message. If acceptable to pregnant women, and demonstrated to be effective, this could be utilised to improve maternal immunisation coverage.
Methods
The researchers identified two hospitals interested in trialing customised video messaging in their antenatal clinics through a larger project aimed at improving uptake of maternal influenza vaccination. Hospital A is approximately 250km from Melbourne with more than 600 births per year and Hospital B is approximately 150km from Melbourne with approximately 1400 births per year.
Senior obstetric and nursing/midwifery staff at the respective health services partnered with the researchers, and a consumer representative to develop the content of the video. These local clinicians also featured in the video. The video contained information related to the potential harms of influenza infection for pregnant women and their infants, the safety and efficacy of influenza vaccine and where pregnant women could receive influenza vaccine in their hospital/ community.
Nebula Health is an Australian digital communications team, led by doctors, that have made over 450 medical patient education videos and delivered those videos directly to patients via different software systems. Nebula Health collaborated on this project to provide technical advice on the script, shoot the videos onsite at the health services, edit the video and send the text message with video link utilising customised third party software.
A text message containing a link to the health service-specific video was sent to all pregnant women booked to give birth at each service. Clicking on the link directed the text recipient to a webpage where they could click ‘play’ to watch the video. The first round of text messages was sent in May 2019. Due to low initial engagement with the first round of text messages, the process was subsequently modified. The modifications included: changing the phone number that the text message came from so that the hospital and doctors were clearly identified within the text message. In addition, to make it easier for women to view the video, the link was modified to connect directly to the video, which then played automatically. The second round of text messages were sent in smaller batches in August 2019 (sent to 50 individuals at a time), to allow view rate to be monitored more frequently and further modification of text messages to be made if required.
A convenience sample of women attending antenatal care at these hospitals was invited to complete a questionnaire to assess the acceptability and impact of the video message intervention. The principal investigator approached women while they were in the waiting room of the antenatal clinics in August and September 2019 and asked whether they had received an influenza vaccine during pregnancy. If so, they were offered the questionnaire.
This project was approved by the Human Research and Ethics Committee at both hospitals.
Results
The first round of text messages was sent to 241 women at Hospital A, and 601 women at Hospital B. Analysis after sending this first round of text messages revealed that very few women viewed the video; two viewers (2/241, 0.8%) at Hospital A, and nine viewers (9/601, 1.5%) at Hospital B. The second round of text messages was sent in August 2019 to 266 women at Hospital A, and 476 women at Hospital B. The number of views at each site increased to 127 views by 60 viewers (60/266, 23%) at Hospital A and 201 views by 121 viewers (121/476, 25%) at Hospital B (Figure 1).
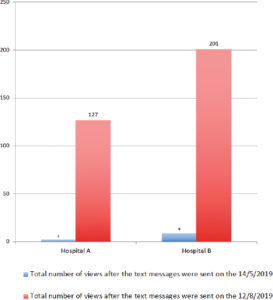
Figure 1: Number of video views.
The questionnaire assessing women’s acceptability of this intervention was completed by 233 pregnant women across both maternity services. Nearly one third (72/233, 31%) recalled receiving the text message, and three quarters of these women (55/72, 76%) reported no problem using the link to the video. Of the 72 women who recalled receiving a text message, 26 (36%) watched the video, and nine of these 26 women (35%) reported being motivated to receive influenza vaccine by the video. Of the remaining 17 participants who reported that the video did not encourage them to have the vaccine, five participants volunteered that they had already received the vaccine. We are unable to clarify the rationale for the remaining 12 participants about why they were not motivated. However, all but one of these participants had already received influenza vaccine at the time of completing the questionnaire.
Of the women who watched the video, the majority agreed that the video was relevant and easy to understand. The majority of them also believed that receiving a personalised video message from the antenatal staff of their maternity service made the health message more relevant to them and agreed that it was convenient to receive health information via text message (Figure 2).

Figure 2: Consumer attitudes toward the video.
Discussion
Our study reports on an innovative way to deliver influenza vaccine recommendation to pregnant women. It demonstrates that providing pregnancy-related health information via text message directly to pregnant women is acceptable, relevant, easy to understand and informs their decision making.
Healthcare provider recommendation is a key driver of influenza vaccine uptake amongst pregnant women.10,11 However, external factors may influence whether influenza vaccination recommendation occurs in a busy clinic environment amongst the multiple other competing priorities of antenatal care. There is a need to develop new methods to facilitate healthcare provider recommendation. Strategies to increase healthcare provider recommendation via automated platforms such as sending text messages have been previously trialled with mixed results.12,13
To the best of our knowledge, our study is the first to use a video developed by local stakeholders to promote maternal influenza vaccine uptake delivered directly to the woman’s mobile phone. The video contributed to women’s decision to be vaccinated in more than a third. Our study differed from the two previous studies in the way in which pregnant women received and viewed the video message. This difference has several advantages. Women in our study received the video via a text message sent to their personal device, so they were able to watch the video at their convenience. This method of delivery also meant that they were able to save the link and view the video again in the future. Another key difference in our study was that we produced and implemented the video message with active involvement from local maternity providers, which was not reported in either of the previous studies.14,15 Personalising the video increased the relevance of the messaging for women and may have contributed to the health impact of this intervention.
Receiving text messages with a link to a video is also less likely to impact the workflow of the antenatal clinic. Whilst incorporating healthcare provider recommendation into routine consultation is essential in promoting vaccine uptake, it may be challenging for some providers to achieve given the busy clinic environment.17 Many pregnant women have competing obstetric, medical, or psychosocial priorities during a consultation. A literature review on the barriers and predictors of maternal vaccine uptake found that some maternity service providers did not have time during their consultation to promote and administer maternal vaccines.18
There were several learning points worthy of note for maternity services who may want to adopt a similar intervention. Firstly, the timing of sending the video is important given the seasonal nature of influenza. Our video was sent in May and August 2019, several months after the seasonal vaccine became available (typically in early April in Australia). Five of the women surveyed indicated that they had already received an influenza vaccine and, therefore, the video did not change their intention to be vaccinated. While we did not specifically ask why women who recalled watching the video were not motivated to be vaccinated, it is possible that they may have already received the vaccine by the time they received the text message. With this in mind, consideration should be given to the optimal timing to deliver this intervention for it to have the most significant impact. Perhaps this strategy could focus on women who have “not yet” been vaccinated during pregnancy despite the vaccines being available. A challenge with this approach is to identify women not yet vaccinated in real-time.
Another key lesson learned from this study is the importance of clearly identifying the hospital and the intention of the text message to avoid the text message being treated as ‘spam’. The text message sent in the first round did not identify the name of the sender, nor an explanation that the link was to a video. A Cochrane review looking at recipients’ perception and experiences of receiving health messages via mobile devices, found that the recipients’ perception of the senders’ identity can influence the trust and perception of the credibility of the text message.19 This review noted that the sender’s phone number should be identifiable and recognisable as being from known health professionals or an official source.20
The importance of this introductory text was demonstrated in the increase in view rate in the second round of text messages in our study. To increase recognition of the text message as being for them and from the hospital, healthcare providers could inform women during their antenatal consultations that they will be sent health information via text message and video during their pregnancy. Furthermore, the same instruction could be added to the patient information package provided to all pregnant women at their initial consultation.
A limitation of our study is that the video was only available in English and may not be suitable for maternity services where there is a high proportion of pregnant women from culturally and linguistically diverse back-grounds. We also did not have a control group to assess the efficacy of this intervention in comparison to other methods to encourage vaccine uptake in pregnant women. The proportion of women who recalled receiving a text message was 31%. Some women who completed the questionnaire may have received the text message several months prior and may have forgotten. Furthermore, the fact the text message was not clearly identifiable as coming from their maternity service in the initial round of messaging may also have contributed to poorer recall. Approximately a third of those who recalled receiving the message reported watching the video. Again while this seems like a low response rate this is comparable to the average open rate (21%) of marketing emails sent to consumers in other industries.20 Similarly, the proportion of women who watched the video is also higher (26/233: 11%) than the ‘click rate’ of marketing emails sent to consumers in other industries (the percentage of users who are sent an email and click on the link attached to email), which is on average 2.6%.20
Conclusion
Healthcare provider recommendation has consistently been demonstrated to be one of the most important factors in improving maternal vaccine uptake. There is a need for novel strategies to facilitate the delivery of this recommendation. Our study demonstrates that delivering a customised vaccine-related health message via video to a large number of pregnant women by means of a text message is an acceptable and potentially persuasive strategy. In the current environment, with an urgent need to ensure maximal coverage of COVID-19 vaccines among the adult population, (particularly pregnant women) it may be timely to leverage the lessons learnt from this project to trial a text message linked video for pregnant women related to the recommendations and safety of COVID vaccines in pregnancy.
Funding
This work was supported by a Better Care Victoria Innovation Fund (IF 18073).
Acknowledgements
The investigators wish to thank the maternity staff members at these two health services who were featured in this video.
References
1. Mertz D, Lo CKF, Lytvyn L, Ortiz JR, Loeb M, Ang LW, et al. Pregnancy as a risk factor for severe influenza infection: An individual participant data meta-analysis. BMC Infect Dis 2019;19(1):1–10.
2. Fell DB, Savitz DA, Kramer MS, Gessner BD, Katz MA, Knight M, et al. Maternal influenza and birth outcomes: systematic review of comparative studies. BJOG 2017;124(1): 48–59.
3. Zaman K, Roy E, Arifeen SE, Rahman M, Raqib R, Wilson E, et al. Effectiveness of maternal influenza immunisation in mothers and infants. N Engl J Med 2008;359(15): 1555–1564.
4. Madhi SA, Cutland CL, Kuwanda L, Weinberg A, Hugo A, Jones S, et al. Influenza vaccination of pregnant women and protection of their infants. N Engl J Med. 2014;371(10):918–931.
5. Nunes MC, Madhi SA. Influenza vaccination during pregnancy for prevention of influenza confirmed illness in the infants: A systematic review and meta-analysis. Human Vaccin Immunother 2018;14:758–766.
6. Maher L, Hope K, Torvaldsen S, Lawrence G, Dawson A, Wiley K, et al. Influenza vaccination during pregnancy: Coverage rates and influencing factors in two urban districts in Sydney. Vaccine 2013;31(47):5557–5564.
7. Regan AK, Mak DB, Hauck YL, Gibbs R, Tracey L, Effler P V. Trends in seasonal influenza vaccine uptake during pregnancy in Western Australia: Implications for midwives. Women and Birth 2016;29(5):423–429.
8. Rowe SLR, Perrett KP, Morey R, Stephens N, Cowie BC, Nolan TM, Leder K, Pitcher H, Sutton B, Cheng AC. Influenza and pertussis vaccination of women during pregnancy in Victoria, 2015–2017. Med J Aust 2019;210(10):454–462.
9. Krishnaswamy S, Cheng AC, Wallace EM, Buttery J, Giles ML. Understanding the barriers to uptake of antenatal vaccination by women from culturally and linguistically diverse backgrounds: A cross-sectional study. Hum Vaccin Immunother. 2018;14(7):1591–1598.
10. Bisset KA, Paterson P. Strategies for increasing uptake of vaccination in pregnancy in high-income countries: A systematic review. Vaccine 2018;36(20):2751–2759.
11. Mohammed H, Clarke M, Koehler A, Watson M, Marshall H. Factors associated with uptake of influenza and pertussis vaccines among pregnant women in South Australia. PLoS One 2018;13(6):1–14.
12. Stockwell MS, Westhoff C, Kharbanda EO, Vargas CY, Camargo S, Vawdrey DK, et al. Influenza vaccine text message reminders for urban, low-income pregnant women: A randomised controlled trial. Am J Public Health. 2014;104.
13. Moniz MH, Hasley S, Meyn LA, Beigi RH. Improving Influenza Vaccination Rates in Pregnancy Through Text Messaging. Obstet Gynecol. 2013;121(4):734–740.
14. Kriss JL, Frew PM, Cortes M, Malik FA, Chamberlain AT, Seib K, et al. Evaluation of two vaccine education interventions to improve pertussis vaccination among pregnant African American women: A randomised controlled trial. Vaccine 2017;35(11):1551–1558.
15. Frew PM, Kriss JL, Chamberlain AT, Malik F, Chung Y, Cortes M, et al. A randomised trial of maternal influenza immunisation decision-making: A test of persuasive messaging models. Hum Vaccin Immunother 2016;12(8):1989–1996.
16. Hussain T, Smith P, Yee LM. Mobile Phone-Based Behavioral Interventions in Pregnancy to Promote Maternal and Fetal Health in High-Income Countries: Systematic Review. JMIR mHealth uHealth. 2020;8(5):e15111.
17. Webb H, Street J, Marshall H. Incorporating immunisations into routine obstetric care to facilitate Health Care Practitioners in implementing maternal immunisation. Hum Vaccin Immunother. 2014;10(4):1114–1121.
18. Lutz CS, Carr W, Cohn A, Rodriguez L. Understanding barriers and predictors of maternal immunisation: Identifying gaps through an exploratory literature review. Vaccine 2018;36(49):7445–7455.
19. Ames H, Glenton C, Lewin S, Tamrat T, Akama E, Leon N, et al. Clients’ perceptions and experiences of targeted digital communication accessible via mobile devices for reproductive, maternal, newborn, child, and adolescent health: a qualitative evidence synthesis (Review). Cochrane Database Syst Rev. 2019;(10).
20. Mailchimps. Average email campaign stats of Mailchimp customers by industry [Internet]. Available from: https://mailchimp.com/resources/email-marketing-benchmarks/

