‘Setting the framework for intelligent apps’
Rahul Chakrabarti, Chandrashan Mahendra Perera
Co-Editors in Chief
Journal MTM 3:2:1, 2014
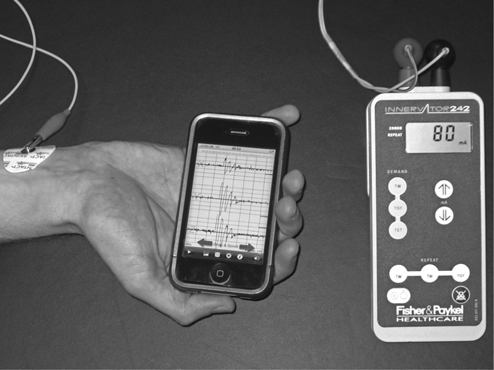
It is with great privilege that we present this second issue of the Journal for the year with a poignant publication on the framework of app development by Marvel et al. Many of our readership audience, who themselves are app developers are overtly aware of the need for closer examination of app quality over quantity. Recent reviews of apps in medical subspecialties have highlighted deficiencies in what is largely an unsolicited market. Issues that have emerged on review of medical apps include scientific accuracy of content, achieving the intended objectives, paucity of peer review/ expert involvement, and consideration of the needs the end-user.1,2 Regulation of medical apps in particular is tantamount given they are readily accessible to a public audience. Thus misleading information or inaccuracies of the app may have ramifications upon individual health directly.
In their timely article Marvel et al summarise the important principles of creating mobile applications. Their ‘ten-step’ framework for app development is conceptualised into four phases: App vision, Creation, Dissemination, and Determining Utility. The authors highlight, using the case study of their own app, the issues and challenges considered at each step of app development. Importantly, this article provides a guideline of aspects for clinicians aspiring to develop clinically useful apps. Critically, the authors remind the audience that whilst development of an app is relatively straightforward, it is the planning and review process that is needs greatest attention. The latter is particularly important for apps that are not required to undergo FDA approval and freely enter an otherwise unregulated market.
The FDA has narrowed its focus primarily to apps which function as medical devices, and as such other apps may be subject to less scrutiny. Nevertheless it is important to understand that many of these apps are still being used by medical professionals to aid in daily practice, and the accuracy and reliability of such apps is still of vital importance. With any new development in the medical field, rigorous testing through scientific processes documented in the literature is necessary, and the use of apps should be no different. Whilst many apps claim to achieve certain goals, it is not without objective testing that a clinician should rely upon these apps, and at the Journal of Mobile Technology in Medicine we encourage developers to show evidence of their app’s claimed benefit.
With the surge in simplicity of app development and accessibility to end-users there is a growing emphasis on regulation. We encourage our audience to consider these logical principles to improve the quality of medical apps rather than mislead the public with increasing mediocrity.
References
1. Cheng NM, Chakrabarti R, Kam JK. iPhone applications for eye care professionals: a review of current capabilities and concerns. Telemed J E Health. Apr 2014;20(4):385–7.
2. Franko OI. Smartphone apps for orthopaedic surgeons. Clinical orthopaedics and related research. Jul 2011;469(7):2042–8.
Read More