Teleophthalmology through handheld mobile devices: a pilot study in rural Nepal
Karen Hong1, Sean Collon2, David Chang3, Sunil Thakalli4, John Welling4, Matthew Oliva4, Esteban Peralta5, Reeta Gurung6, Sanduk Ruit6, Geoffrey Tabin1,4, David Myung1,7, Suman Thapa6
1Byers Eye Institute, Stanford University School of Medicine
2Vanderbilt University School of Medicine
3Los Altos Eye Physicians, Los Alto, CA
4Himalayan Cataract Project
5University of Florida School of Medicine
6Tilganga Institute of Ophthalmology, Kathmandu, Nepal
7Division of Ophthalmology, Veterans Affairs Palo Alto Health Care System, Palo Alto, CA
Corresponding Author: suman.thapa@tilganga.org
Journal MTM 8:1:1–10, 2019
Background: To compare screening referral recommendations made by remotely located ophthalmic technicians with those of an ophthalmologist examining digital photos obtained by a portable ophthalmic camera system powered by an iOS handheld mobile device (iPod Touch).
Methods: Dilated screening eye exams were performed by ophthalmic technicians in four remote districts of Nepal. Anterior and posterior segment photographs captured with a Paxos Scope ophthalmic camera system attached to an iPod Touch 6th generation device were uploaded to a secure cloud database for review by an ophthalmologist in Kathmandu. The ophthalmic technicians’ referral decisions based on slit-lamp exam were compared to the ophthalmologist’s recommendation based on the transmitted images.
Results: Using the transmitted images, the ophthalmologist recommended referral for an additional 20% of the 346 total subjects screened who would not have been referred by the ophthalmic technician. Of those subjects, 34% were referred to the retina clinic. Conversely, among the 101 patients referred by the technician, the ophthalmologist concurred with the appropriateness of referral in more than 97% of cases but thought eight (2.8%) of those patients had variants of normal eye pathology.
Conclusion: An ophthalmologist who reviewed data and photos gathered with the mobile device teleophthalmology system identified a significant number of patients whose need for referral was not identified by the screening technician. Posterior segment pathology was most frequently found by the remote reader and not by the technician performing dilated slit lamp examinations. These results are promising for further clinical implementation of handheld mobile devices as tools for teleophthalmic screening in resource-limited settings.
Keywords: telemedicine, rural population, ophthalmology, referral and consultation, global health
Introduction
The utility of eye screening examinations using portable mobile devices such as smartphones and tablets in developing countries is still largely unexplored. However, several publications1 and systematic reviews2,3 suggest that teleophthalmology can provide cost effective ophthalmic assessments comparable in quality to an in-person exam4–8. This can be feasible even in the most rural corners of the world as the rate of mobile phone usage and wireless internet connectivity is increasing fastest in low and middle income countries to near ubiquitous levels, often surpassing access to clean water and food.9,10 The growing availability of mobile devices with wireless connectivity and high quality in-phone camera technology combine to make mobile device-based teleophthalmology a promising diagnostic tool in resource-limited settings.
The first point of medical contact for a patient with eye complaints in rural Nepal is often at their nearest community eye center (CEC) where they are evaluated by ophthalmic technicians who have completed at least three years of basic science, ophthalmic theory, and clinical practice training. Technicians learn through on-the-job apprenticeship from senior technicians how to conduct eye exams similar to those performed in a developed country’s emergency room with a tonometer, slit lamp, and visual acuity chart. They are educated on treating basic eye complaints like corneal abrasions and refractive error and trained to identify candidates for cataract surgery and which patients to refer. The main eye hospital in the capital city of Kathmandu is the only location where ophthalmic sub-specialty and surgical services are offered. Rural patients must frequently travel hundreds of kilometers to obtain subspecialty, surgical, or postoperative care. The arduous journey by car, bus, or foot is often medically necessary; however, many routine follow-up visits or non-urgent consultations could also be managed at the nearest CEC.11,12
In this study, the Paxos Scope13,14 teleophthalmology platform (Fig 1) was implemented in select remote CECs of the Tilganga Institute of Ophthalmology (TIO) Health Care System in Nepal to characterize referral patterns based on routine exam and photos from a specialized portable mobile device. TIO is the largest provider of ophthalmic care in Nepal, including cataract surgery camps, hospital-based surgery, subspecialist consultation, medical residency training, and research. CECs are permanent rural satellite locations of TIO, staffed by non-ophthalmologists using slit lamps to screen for eye disease warranting subspecialty referral. These differ from mobile itinerant screening camps that are periodically conducted within different remote villages; the latter primarily use visual acuity and flashlight exams to screen for cataracts requiring surgery at a future mobile cataract surgical camp.

Figure 1: Upper: An ophthalmologist using the Paxos Scope mobile ophthalmic camera by Verana Health (San Francisco, CA, USA). Lower: The Paxos Scope components: 1-Flexible lens adaptor, 2-Anterior Adaptor, 3-Posterior Adaptor, 4-20D Lens, 5-iOS device by Apple, Inc. (Cupertino, CA, USA).
Previous studies showed that excellent high-quality images could be taken with both an older15 and current16 version of the Paxos Scope. It is a medical device attachment that requires about six hours of supervised practice screening per day for four days to become proficient.15 This portable technology enables an accurate diagnosis to be made remotely. A validation study suggested that high definition photos viewed on a mobile device are comparable in quality to those viewed on a desktop17, enabling supervising ophthalmologists to provide real-time feedback to the field while attending to their clinic duties.
Teleophthalmology consultations with TIO ophthalmologists in Kathmandu could potentially provide rural CEC staff with additional support in making referral decisions. Properly identifying patients that should see an ophthalmologist targets care and reduces missed diagnoses. The objective of this study is to assess the impact of the Paxos teleophthalmology platform at four Nepali CECs in making referral decisions.
Methods
Research adhered to the tenets of the Declaration of Helsinki and was performed ethically in accordance with the Institutional Review Board at the Tilganga Institute of Ophthalmology. All image acquisition and transmittal was handled with strict attention to the confidentiality of personal data in accordance with the Data Protection Act of 1998 and Access to Health Records of 1990. Verbal informed consent was obtained from subjects and the study was conducted in a Health Insurance Portability and Accountability Act (HIPAA)-compliant manner.
Over a four-day period, Community Eye Center ophthalmic technicians in the Nepali districts of Ramechhap, Jiri, Dolakha, and Charikot were trained by authors JW, EP, and MO on the use of the Paxos Scope, a 510k-registered ophthalmic camera system (commercialized by DigiSight Technologies, which is now Verana Health, San Francisco, CA, USA). This small, portable device allows for magnified anterior segment and fundus photography (Fig 2) when attached to an iOS mobile device (iPod Touch, 6th generation, Apple, Inc, Cupertino, CA, USA). Secure cloud based storage of all patient information was accomplished using HIPAA compliant Paxos software, available on the iOS App Store for all iOS devices.
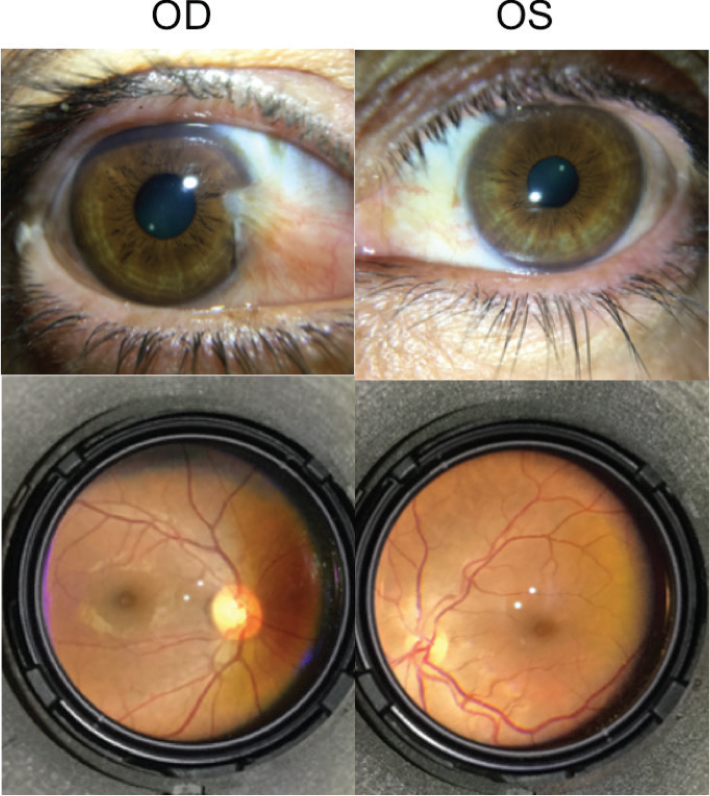
Figure 2: Anterior and posterior segment images taken with the Paxos Scope of the right eye (OD) and the left eye (OS).
Patients giving informed consent were enrolled in the study during their normal CEC appointment. The participant first underwent nonmydriatic anterior photography of both eyes with the mobile device attached to a Paxos Scope anterior adaptor. The Paxos mobile device application was used to focus and capture all photos and served as the HIPAA-compliant patient medical information and image repository. The adaptor consisted of a macro lens that slides in front of the mobile phone’s camera lens to provide the right amount of magnification to capture a photo of the anterior segment of the eye when the mobile device and adaptor unit is held a few centimeters from the participant’s eye. An LED light on the adapter provided uniform lighting for adequate image detail. Pressing down on the mobile device screen in the Paxos application captured multiple photos. The best in-focus photos were saved into the patient’s virtual chart, per the ophthalmic technician’s discretion. The technician then conducted their ophthalmic exam as usual, which included visual acuity, refraction, and dilated slit lamp examination (using a 90 D lens). The ophthalmic technician recorded their binary decision (yes/no) regarding whether or not the participant warranted referral to TIO. The decision was based on identified pathology that could not be treated at a CEC such as glaucoma or poor visual acuity uncorrected by refraction. Next, a lens-holding adapter containing a 20D indirect ophthalmoscopy examination lens was locked into place to the anterior attachment with the proper alignment and working distance to obtain the fundus photo of each eye. During posterior segment photography, the macro lens was slid to one side to prevent obstruction of the mobile device camera lens. The 20D lens was brought close to the participant’s eye, then using the view on the screen of the mobile device, the technician ensured the retina was in focus and filled the image capture frame before image capture. Of note, mature cataracts were not referred because these patients were given information on the next local mobile surgical camp. The medical information and photos could either be viewed on the Paxos application or online on a HIPAA-compliant password-protected website.
A patient’s profile in the Paxos application was deemed complete if it contained anterior and posterior segment photos of both eyes, as well as visual acuity. The technicians chose to record other elements of their normal exam as they thought relevant to the patient’s case. One ophthalmologist at TIO (author ST) served as the blinded photo grader. Along with the photos, the study reviewed additional patient information including visual acuity, refraction, and IOP to determine whether the patient could be managed at the local CEC, or whether they should be transported to TIO for care and evaluation by an ophthalmologist. The decision to refer was based on the identification of ocular pathology that could be treated or needed to be monitored by a subspecialist, like a retinal detachment or advanced diabetic retinopathy. ST also determined the subspecialty clinic to which the patient should be referred, which the ophthalmic technicians were not asked to assess.
Statistical analysis was performed in STATA 15. Descriptive data were presented as means and standard deviations, or counts and percentages as appropriate. The primary outcome measure was a calculated unweighted Cohen’s kappa coefficient for inter-rater agreement on referral status. The ophthalmologist’s referrals were categorized by referral subspecialty. Discrepancy in the referring decisions between the ophthalmologist and the rural technicians were analyzed with respect to disease type. All cataract clinic referrals made by the ophthalmologist were categorized as “no referral” because, although technicians and ophthalmologists agreed regarding the need for cataract surgery, technicians generally recommended that these patients return to the CEC in the next several months to attend a local surgical camp, rather than traveling to Tilganga. These surgical camps are organized and conducted by TIO ophthalmologists, and happened at least once every year at each of Tilganga’s sixteen CECs.
Results
Over a ten month study period, 346 total patients were enrolled in the study from the Ramechhap (n=126), Charikot (n=55), Dolakha (n=124), and Jiri (n=41) CECs. Of those, 54% were male and the mean age was 63 years old (Table 1). All recruited subjects were included in this study, with 72.5% having “complete” teleophthalmology exams, including basic health demographic information and bilateral anterior segment and fundus photos (total of at least 4) stored in the Paxos application. The technician and ophthalmologist made the same referral decision 77.4%, not 77.5% of the time (Table 2), resulting in a Cohen’s unweighted kappa of 0.56 (95% CI of 0.46- 0.65), which is suggestive of moderate agreement.
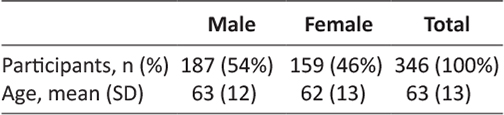
Table 1: Demographics at the Community Eye Centers in Ramechhap, Jiri, Dolakha, and Charikot districts
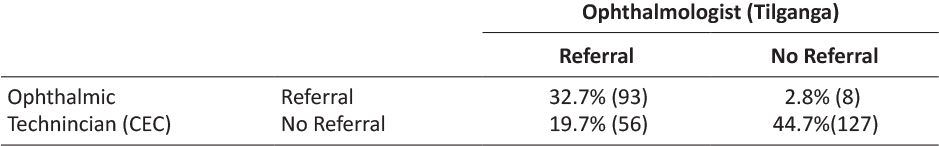
Table 2: Referral rates from Community Eye Centers to Tilganga Institute of Ophthalmology Health Care System
Among those patients that were not referred by the technician, the ophthalmologist identified 56 subjects (19.7%) that needed referral to TIO for evaluation or care. The TIO subspecialty clinics to which patients were referred based on photo examination by the ophthalmologist were retina (33.9%), glaucoma (30.4%), general clinic (17.9%), neuro-ophthalmology (5.4%), cornea (1.3%), and oculoplastics (1.3%) (Fig 3). Of the 101 patients referred to TIO by the technician, the ophthalmologist felt that referral was unnecessary for eight (2.8%) because the eyes were variants of normal in all cases. Reasons that the ophthalmogist wanted to see a patient that the technician did not refer included asymmetrical cupping, elective pterygium, and left macular hole (Fig 4) that were either missed by the ophthalmic technician or they did not feel warranted specialist referral.
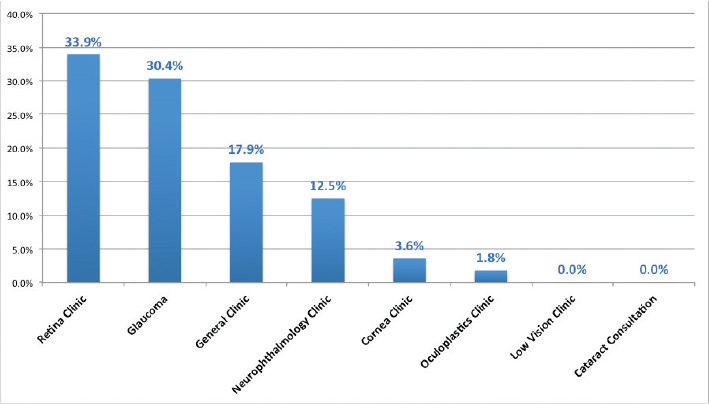
Figure 3: Percentage of participants by referred subspecialty here reviewing ophthalmologist referred and ophthalmic technician decided not to refer.
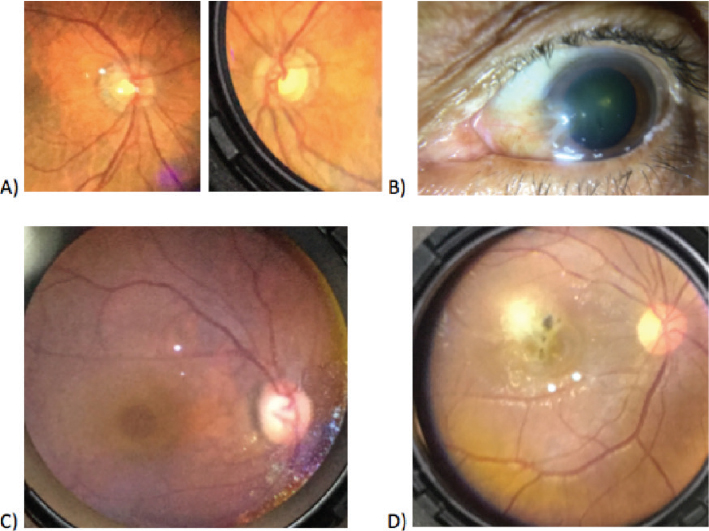
Figure 4: Examples of ocular pathology as captured on anterior and posterior segment photographs with the Paxos Scope. A) Asymmetrical cupping in fundus photos of the right eye (left side) and left eye (right side) B) Pterygium located on the medial portion of the left eye of the subject C) Macular hole in the fundus photo of a right eye.
Out of all the TIO referrals that the ophthalmologist decided to make, the sub-specialty referral trends were similar to those described above that the ophthalmic technicians made, with retina (43.8%), glaucoma (26.7%), general clinic (17.1%), neuro-ophthalmology (7.6%), cornea (1.9%), and oculoplastics (1.9%), and low vision clinic (0.9%) as the distribution of referrals.
Of note, 18.4% of the ocular photos were missing, which meant 27.5% of the participants had to be excluded from analysis because they had an incomplete chart, per the analysis inclusion criteria definition. Out of all the participants with missing photos, 40.4% had only posterior photos missing, 14.0% had only anterior photos missing, 13.2% had a combination of anterior and posterior photos missing, and 32.5% had all photos missing. Of the participants that had all photos missing, 89.2% came from Jiri district.
Discussion
The TIO CEC ophthalmic technicians do an outstanding job in spite of limited resources and direct oversight—highlighted by the fact that remote eye MD readers agreed 77.4% of the time with them. This is a testament to the excellent training they have received through TIO and their conscientious work in the field, in particular in screening for cataracts and identifying “normal” exams as well as anterior segment pathology. The technicians indicated after study completion that they missed some posterior pole pathology because they did not have previous experience identifying them, but with feedback through the Paxos fundus photographs and telecommunication with the ophthalmologist, they have enhanced their arsenal of knowledge. They did not refer some pathology like pterygiums because it did not clinically impact the patient’s quality of life, which the remote ophthalmologist could not take into account. Therefore it is important to acknowledge that the technician is crucial to patient-centered care because the clinical context of the whole patient cannot always be fully be captured in a telelophthalmic photograph.
The results from this study also suggest that mobile device teleophthalmology could serve as a useful adjunct to the screening exams performed by ophthalmic technicians in CECs. Use of the Paxos teleophthalmology system in four community eye centers in Nepal did improve the percentage of patient identified with referable pathology. Of the patients screened, nearly 20% merited referral for conditions that were not identified via technician slit lamp examination at the CEC. Disagreements about whether or not to refer a patient were most frequently related to retinal or glaucoma pathology, while referral-warranted anterior segment pathology was rarely missed. When a technician did decide to refer a patient to TIO, the ophthalmologist almost always agreed. Therefore, technician referral decisions were characterized by few false positives, but a higher rate of false negatives. Using a camera-enable mobile device may be a way to capture all necessary referrals to TIO. As technicians learn from feedback through synchronous or asynchronous communication with an ophthalmologist, this may help lower the rate of presumed false negatives.
In addition to detecting significant ocular pathology that might otherwise be missed, mobile device teleophthalmology has many other potential benefits. From the patient perspective, the reduced need for travel provides convenient access to healthcare; patients appreciated the convenience of having remote digital evaluation by an ophthalmologist without having to travel to Kathmandu. In fact, one study reports similar patient satisfaction scores whether their exam was done in-person or through teleophthalmic means.18 The technicians appreciated the opportunity to evaluate the photos, although they were not allowed to change their referral decision for purposes of the study. Lastly, obtaining the feedback and diagnoses from the reviewing ophthalmologist provided significant continued on-the-job training to the technician on more subtle pathology, particularly in the posterior segment. The Paxos System provides a posterior pole photograph of the fundus which is similar to an examiner’s view during indirect ophthalmoscopy, a rare luxury as part of the rural ophthalmic exam something that is typically not available in settings outside of an eye clinic, and particularly in rural areas.
There are numerous studies evaluating the rural use of teleophthalmology using table-top cameras and their outcomes in India19–21, Australia,12, Spain22, USA23–25, Kenya26, China27, Greece28, Brazil,11 and the UK.29 Most research has been done with diabetic retinopathy screening, for which there is a general consensus that teleophthalmology efforts increase the number of screened patients without sacrificing quality of care or visual outcomes.21,29,30 Comparing data from the Beijing Eye Public Health Care Project to our own findings, subspecialty referrals had similar trends (excluding cataract surgery due to Nepal’s unique local cataract camps): retinal disease (including macular and retinopathy changes) was the most commonly detected pathology, followed by glaucomatous optic neuropathy.27 In a study conducted in rural Brazil, teleophthalmology was highly specific and sensitive in detecting urgent eye conditions.11 An internet-based initiative in rural Australia found that using an online photographic repository helped to triage ocular emergencies remotely.12 The low-cost, portability, and wireless connectivity inherent to a handheld, mobile device-based teleophthalmology system like Paxos Scope expands the reach of expert ophthalmic care to remote locations similar to the CECs included in this study.
Moreover, because the iPod Touch 6th generation has an 8 megapixel camera that is very similar to the iPhone 6, the results from this study can be directly translatable to the use of Paxos Scope with the iPhone 6 or higher. The primary reason that the iPod Touch was used in this study was cost—at a price point (in 2016) of $199 per unit, it was less than a one-third the retail cost of the iPhone 6. Thus, we were able to obtain several units for this study and distribute them to the CECs. We also chose this device because it did not have cellular connectivity. Although cellular connectivity is available in rural Nepal, it is typically lower in bandwidth and more importantly, requires a data plan that charges by the megabyte. Because the images being taken were large in both size and quantity, we decided to avoid the challenges and issues related to the setting up of contracts, cellular data plans, recurring charges, and overages and rely strictly on WiFi connectivity. This decision provided many logistical and budgetary advantages, but also revealed some regional inconsistencies.
This study had several limitations. First, it relied on evaluations by four different technicians whose training and diagnostic skills may have differed. Second, more than a quarter of the participants had missing photos from their chart and therefore could not be included in analysis. Reasons for missing data included inability of the patient to stay still long enough to capture a photo, poor view into the back of the eye because of a cataract or other obstruction, and inability to upload into the digital cloud in certain situations due to inconsistent WiFi connectivity in the field. Jiri district accounted for most of the participants that did not have any photos because of uploading issues and lack of Wifi access. Even though the technician would capture the correct images, the photographs had to be manually uploaded to a desktop computer because of poor Wifi access and the photographs failed to transfer. This was not an issue at the three other sites because they uploaded their photographs through reliable and stable Wifi. This issue has been resolved with the newer version of the Paxos application through an automatic caching and uploading process. Thus, the data may be biased toward healthier patients who can tolerate sitting still for longer, and those that are in areas that are more developed with strong and stable WiFi.
Third, and perhaps most significantly, there are many subjective factors that affect the referral decision by both technician and ophthalmologist. For instance, a technician may not refer some patients with recognized pathology due to an understanding of a patient’s inability to afford the travel. A remote ophthalmologist may have changed their referral decision if they could have further queried the patient about their main concern as well as their past medical and social history. Decisions could have affected the results either way. In addition, it is possible that some of the WiFi connectivity issues encountered may have been avoided if cellular data plans were used in concert as is often done on consumer cell phones that alternate between cellular and WiFi when the latter is available, in particular for data-intensive transfer activity such as photo uploads to cloud storage. Nonetheless, we feel that the results strongly suggest a role for mobile device-based teleophthalmology systems as they provide more patients the opportunity to access healthcare.
Future studies should focus not just on the ability to properly refer and manage rural patients, but also on outcomes. The correlation between the Paxos photographs and the in-person ophthalmologist findings should be studied. The next step of future studies is to track each patient’s care to identify who required specialty treatment at TIO. Finally, more than 100,000 patients are annually screened without slit lamps at community-based camps, and this dwarfs the number of patients seen at the CECs. These screening camps refer thousands of patients for cataract surgery at CEC based surgical camps. However, very little is known about ocular co-morbidies such as glaucoma or retinopathy. The utility of Paxos Scope should be investigated for these screening camps as well.
In summary, the results reported in this study suggest strongly that mobile device teleophthalmology has the potential to improve patient care in rural Nepal by improving and increasing detection of posterior segment pathology. Previously, the ophthalmic technician fundus screening was performed using only the 90D slit lamp biomicroscopy. Due to its cost-effective, portable, hand-held design, the ophthalmic camera and teleophthalmology system presented here can be obtained and placed in multiple locations within a health care system. In doing so, TIO has the potential to expand the reach of remote ophthalmologists to rural satellite locations.
Conclusions
Based on the results of this study, mobile device teleophthalmology could play an important role as an adjunct to patient care already being delivered by TIO technicians in CEC settings of rural Nepal. Use of a mobile device-based ophthalmic camera improves detection of ocular pathology, particularly that of the posterior segment, and therefore has potential to improve patient management and patient outcomes. Although our study was only in TIO CECs, it is reasonable to suspect that similar results might also be obtained in other rural communities that are served by health care workers trained in the ophthalmic exam. It is likely that mobile device-based ophthalmic cameras would be beneficial tools for teleophthalmology in a number of rural and developing settings due to their excellent portability, durability, affordability, and their ability to take high quality images.
Acknowledgements
The authors would like to acknowledge the ASCRS Foundation who provided funds to carry out this study, as well as the Himalayan Cataract Project and the Moran Eye Center for supporting author JW during his international fellowship. The authors would also like to acknowledge Digisight Technologies for their support.
Declarations
Karen Hong has received a research grant from the Mary Duke Biddle Clinical Scholars Program and Dr. David Myung holds a patent for the Paxos Scope. Digisight Technologies (now Verana Health) provided the Paxos Scope technology for this study. All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and have no other relationships or activities that could appear to have influenced the submitted work.
References
1. Sreelatha OK, Ramesh SV. Teleophthalmology: improving patient outcomes? Clin Ophthalmol. 2016;10:285–95. ![]()
2. Labiris G, Panagiotopoulou E, Kozobolis VP. A systematic review of teleophthalmological studies in Europe. Int J Ophthalmol. 2018;
3. Tan IJ, Dobson LP, Bartnik S, Muir J, Turner AW. Real-time teleophthalmology versus face-to-face consultation: A systematic review. J Telemed Telecare. 2017;23(7):629–38. ![]()
4. Toy BC, Myung DJ, He L, Pan CK, Chang RT, Polkinhorne A, et al. Smartphone-Based Dilated Fundus Photography and Near Visual Acuity Testing As Inexpensive Screening Tools To Detect Referral Warranted Diabetic Eye Disease. Retina. 2016;36(5):1000–8. ![]()
5. Toy BC, Myung DJ, He L, Pan CK, Chang RT, Polkinhorne A, et al. Simple, Low-Cost Smartphone Adapter for Rapid, High Quality Ocular Anterior Segment Imaging: A Photo Diary. Indian J Ophthalmol. 2014;3(1):285–95. ![]()
6. Johnston K, Kennedy C, Murdoch I, Taylor P, Cook C. The cost-effectiveness of technology transfer using telemedicine. Health Policy Plan. 2004;19(5):302–9. ![]()
7. Mitchell J. Increasing the cost-effectiveness of telemedicine by embracing e-health. J Telemed Telecare. 2000;6(1_suppl):16–9. ![]()
8. de la Torre-Díez I, López-Coronado M, Vaca C, Aguado JS, de Castro C. Cost-Utility and Cost-Effectiveness Studies of Telemedicine, Electronic, and Mobile Health Systems in the Literature: A Systematic Review. Telemed e-Health. 2015;21(2):81–5. ![]()
9. Bastawrous A, Hennig BD, Livingstone I. mHealth Possibilities in a Changing World. Distribution of Global Cell Phone Subscriptions. J Mob Technol Med. 2013;2(1):22–5. ![]()
10. Bastawrous A. Increasing access to eye care… there’s an app for that. Peek: smartphone technology for eye health. Int J Epidemiol. 2016;(May):1040–3. ![]()
11. Ribeiro AG, Rodrigues RAM, Guerreiro AM, Regatieri CVS. A teleophthalmology system for the diagnosis of ocular urgency in remote areas of Brazil. Arq Bras Oftalmol. 2014;77(4):214–8. ![]()
12. Kumar S, Yogesan K, Hudson B, Tay-Kearney ML, Constable IJ. Emergency eye care in rural Australia: Role of internet. Eye. 2006;20(12):1342–4. ![]()
13. Myung D, Jais A, He L, Blumenkranz MS, Chang RT. 3D Printed Smartphone Indirect Lens Adapter for Rapid, High Quality Retinal Imaging. J Mob Technol Med. 2014;3(1):9–15. ![]()
14. Myung D, Jais A, He L, Chang RT. Simple, Low-Cost Smartphone Adapter for Rapid, High Quality Ocular Anterior Segment Imaging: A Photo Diary. J Mob Technol Med. 2014;3(1):2–8. ![]()
15. Ludwig CA, Newsom MR, Jais A, Myung DJ, Murthy SI, Chang RT. Training time and quality of smartphone-based anterior segment screening in rural India. Clin Ophthalmol. 2017;11:1301–7. ![]()
16. Ludwig C, Murthy S, Pappuru R, Jais A, Myung D, Chang R. A novel smartphone ophthalmic imaging adapter: User feasibility studies in Hyderabad, India. Indian J Ophthalmol. 2016;64(3):191–200. ![]()
17. Lamirel C, Bruce BB, Wright DW, Newman NJ, Biousse V. Nonmydriatic digital ocular fundus photography on the iPhone 3G: The FOTO-ED study. Arch Ophthalmol. 2012;130(7):939–40. ![]()
18. Tuulonen A, Ohinmaa A, Alanko HI, Hyytinen P, Juutinen A, Toppinen E. The application of teleophthalmology in examining patients with glaucoma: A pilot study. Vol. 8, Journal of Glaucoma. 1999. p. 367–73. ![]()
19. John S, Premila M, Javed M, G V, Wagholikar A. A Pilot Study to Improve Access to Eye Care Services for Patients in Rural India by Implementing Community Ophthalmology through Innovative Telehealth Technology. Stud Health Technol Inform. 2015;214(41):139–45.
20. Ramon R, Bhojwani DN, Sharma T. How accurate is the diagnosis of diabetic retinopathy on telescreening ? The Indian scenario. 2014;1–5.
21. Murthy KR, Murthy PR, Kapur A, Owens DR. Mobile diabetes eye care: Experience in developing countries. Diabetes Res Clin Pract. 2012;97(3):343–9. ![]()
22. Rodríguez Villa S, Alonso Álvarez C, de Dios del Valle R, Salazar Méndez R, Cuesta García M, Ruiz García MJ, et al. Five-year experience of tele-ophthalmology for diabetic retinopathy screening in a rural population. Arch la Soc Española Oftalmol (English Ed. 2016;91(9):426–30. ![]()
23. Maa AY, Wojciechowski B, Hunt KJ, Dismuke C, Shyu J, Janjua R, et al. Early Experience with Technology-Based Eye Care Services (TECS): A Novel Ophthalmologic Telemedicine Initiative. Ophthalmology. 2017;124(4):539–46. ![]()
24. Chin EK, Ventura B V., See K-Y, Seibles J, Park SS. Nonmydriatic Fundus Photography for Teleophthalmology Diabetic Retinopathy Screening in Rural and Urban Clinics. Telemed e-Health. 2014;20(2):102–8. ![]()
25. Jani PD, Forbes L, Choudhury A, Preisser JS, Viera AJ, Garg S. Evaluation of diabetic retinal screening and factors for ophthalmology referral in a telemedicine network. JAMA Ophthalmol. 2017;135(7):706–14. ![]()
26. Kherani I, Gichuhi S, Damji K, Nyenze M, Kiage D. The muranga teleophthalmology study: Comparison of virtual (teleglaucoma) with in-person clinical assessment to diagnose glaucoma. Middle East Afr J Ophthalmol. 2013;20(2):150–7. ![]()
27. Xu L, Jonas JB, Cui TT, You QS, Wang YX, Yang H, et al. Beijing eye public health care project. Ophthalmology. 2012;119(6):1167–74. ![]()
28. Labiris G, Fanariotis M, Christoulakis C, Petounis A, Kitsos G, Aspiotis M, et al. Tele-ophthalmology and conventional ophthalmology using a mobile medical unit in remote Greece. J Telemed Telecare. 2003;9(5):296–9. ![]()
29. Sim DA, Mitry D, Alexander P, Mapani A, Goverdhan S, Aslam T, et al. The Evolution of Teleophthalmology Programs in the United Kingdom: Beyond Diabetic Retinopathy Screening. J Diabetes Sci Technol. 2016;10(2):308–17. ![]()
30. Salongcay RP, Silva PS. The Role of Teleophthalmology in the Management of Diabetic Retinopathy. Asia-Pacific J Ophthalmol. 2018;7(1):17–21. ![]()

