mHealth Can Activate Patients to Discuss Hepatitis C Screening with Physicians
John B. Kellogg, BA1, Jessica D. Lee2, Daniel R. Murphy, MD, MBA1,3, Monisha Arya, MD, MPH1,3
1Baylor College of Medicine, One Baylor Plaza, Houston, TX 77030, USA;
2Rice University, 6100 Main St, Houston, TX 77005, USA;
3Center for Innovation in Quality, Effectiveness and Safety, Michael E. DeBakey VA Medical Center, 2002 Holcombe Blvd, Houston, TX 77030, USA;
Corresponding Author: Kellogg@bcm.edu
Journal MTM 8:1:20–28, 2019
Background: Despite the prevalence of hepatitis C virus (HCV) and the availability of effective treatments, HCV screening remains suboptimal, in part due to primary care physicians’ (PCPs) unawareness of and discomfort discussing HCV risk factors. Patient-facing text message campaigns may overcome these barriers by empowering patients to initiate screening discussions with their PCPs.
Aims: The objectives were to evaluate a patient-facing text message campaign in terms of (1) feasibility, (2) acceptability, and (3) impact on patient-PCP discussions about HCV screening.
Methods: Primary care patients were recruited to receive either an HCV text message, which contained HCV information and a prompt to discuss HCV with their PCPs, or a calcium control text message. Forty minutes before their appointments, participants were sent their assigned text message. Participants were then called for an evaluation of the text message campaign.
Results: Of 185 patients called, 38 enrolled and completed the study. Participants who were sent an HCV text message (n=25) were significantly more likely to initiate a conversation with their PCPs about HCV screening than participants sent a calcium control text message (n=13) (p=0.008). Thirty-two (82%) participants liked receiving a health-related text message (88% in the HCV group; 70% in the control group).
Conclusions: A patient-facing HCV text message campaign shows promise as a novel method to activate primary care patients to initiate HCV screening discussions with their PCPs. This campaign may help educate patients about the importance of HCV screening, overcome physician barriers to screening, and, ultimately, help control the HCV epidemic.
Keywords: hepatitis C, text messaging, physician-patient relations, preventive health services, primary health care
Introduction
Hepatitis C remains a hidden epidemic in at-risk populations
Hepatitis C virus (HCV) afflicts approximately 3 million Americans and is the leading cause of liver disease in the United States.1 The U.S. Centers for Disease Control and Prevention (CDC) and the U.S. Preventive Services Task Force (USPSTF) recommend HCV screening for many at-risk populations, including the 1945 to 1965 birth cohort (“baby boomers”).2,3 Despite longstanding HCV screening recommendations and the success of oral direct acting antivirals (DAAs), which can reverse the natural progression of HCV, 45-85% of people with HCV are unaware of their infection because they are asymptomatic and/or untested.4 Among baby boomers, who make up 75% of those infected with HCV5 only 13.8% have been screened.6
Primary care physicians are not routinely screening for HCV and face barriers to do so
While primary care physicians (PCPs) are seen as critical facilitators to increasing HCV screening rates,7 they are struggling to make screening routine. Few PCPs conduct regular assessments of HCV risk factors,8 and, of those who do, even fewer screen these at-risk patients.9 One barrier to screening is a lack of time necessary to assess HCV risk factors.7 Another barrier is knowledge of risk factors; some PCPs are unclear about the at-risk populations needing HCV screening and uncomfortable asking patients about their risk factors.10,11
Text messages may empower patients to overcome PCP HCV screening barriers
According to the Pew Research Center, 95% of Americans own a mobile phone12 and over three-quarters of them send and receive text messages.13 Text messaging is the most used mobile phone feature,14 and health interventions can take advantage of this inexpensive, broad access to patients. Furthermore, text messages can be personalized to enhance effectiveness.15 Studies have found that patients are receptive to receiving health reminders by text message and that text messages can be effective for disease prevention interventions.16–18 For HCV in particular, Levine et al. reported 96% of patients at their clinic would be receptive to receiving a text message encouraging HCV screening19. Moreover, 71% of PCPs surveyed by Thomson et al. thought HCV screening would improve if patients were provided education on HCV;7 thus, patient-centered text messages could help PCPs improve their HCV screening practices by educating patients about HCV. Text messages may also empower patients to ask for the HCV test. According to our previously published health campaign push-pull model, personalized text messages that contain information on disease prevention and recommend further action may “push” patients to “pull” their physician into a health discussion.20 For PCPs who are uncomfortable discussing HCV screening, or who are unfamiliar with risk factors and screening guidelines, a patient-facing, personalized text message campaign may help overcome physician-level barriers.
Study Objective
Although several studies have evaluated physician knowledge and perspectives on HCV screening, studies on patient-centered HCV screening campaigns are limited. The aims of our pilot study were to (1) determine the feasibility of recruiting patients for a mobile health text message campaign, (2) gauge the acceptability of health-related text messages and (3) assess the impact of a campaign on empowering patients to discuss HCV screening with their PCP.
Methods
Study Design
Text Message Content Development
In spring 2017, research staff approached community members at local venues (e.g., grocery stores, cafeterias, etc.) to assess their HCV knowledge and to ask for suggestions on content for an HCV screening campaign. Based on these discussions, the research staff drafted text messages with HCV information and again approached community members to rank their preference of message content. The themes of the highest-ranked text messages were selected by the research staff to be incorporated into the final text message content for the present study (see Table 1).
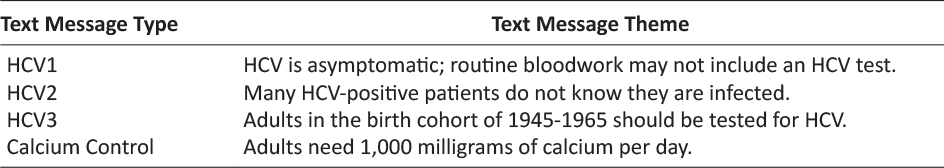
Table 1: Text Message Themes
Each finalized text message began with the participant’s name, included HCV information according to one of the three HCV themes, and ended with a prompt to ask the PCP about HCV screening. To further personalize the text message, the name of the participant’s PCP was included. The research team also created a control text message, which similarly included the participant’s name and PCP’s name, but instead contained information about calcium supplementation.
Participant Recruitment & Enrollment
Patients were recruited from an academic private practice primary care clinic that serves predominately insured patients in Houston, TX. Staff from the study clinic provided the research team with a list of patients who had primary care appointments within the upcoming week. This list included the patient’s name, phone number, PCP’s name, and appointment date and time. From July 7 to August 16, 2017, the research staff called patients at least two business days before their appointment date, with a second call at least one business day before their appointment if they did not answer the initial recruitment call. Patients were provided with a brief description of the study, outlining that participants would receive a text message before their appointment, as well as a phone call after their appointment for a post-text message evaluation survey. The research staff then provided interested patients with more details of the study and screened for eligibility. The eligibility criteria were (1) over the age of 18, (2) English-speaking, (3) own a cell phone and read text messages, and (4) plan to attend their upcoming appointment. The research staff read the consent form to interested and eligible patients; patients that provided verbal consent were then enrolled. To reduce the likelihood of patients failing to answer a post-message follow-up call from an unfamiliar number, we provided the study cell phone number and elicited a preferred date and time to call back. To assess the feasibility of recruitment and retention for this text message campaign study, the research team maintained records of patient recruitment, enrollment, and completion of the study. This study protocol (H35157) was approved by the Baylor College of Medicine Institutional Review Board; participants gave informed consent before taking part.
Text Message Campaign Delivery
Study participants born between 1945 and 1965 were assigned, in order of enrollment, to receive either HCV1, HCV2, HCV3, or calcium control (see Table 1). All other study participants (those not born between 1945 and 1965) were assigned, in order of enrollment, to receive either HCV1, HCV2, or calcium control. These participants were never assigned the HCV3 text message that contained message content targeting the 1945-1965 birth cohort. Forty minutes before a participant’s appointment, the research staff sent the participant his/her assigned text message, substituting in the participant’s name and PCP’s name. Messages were individually typed and sent from the study cell phone.
Post-Text Message Evaluation Surveys
After their appointments, participants were called to determine the acceptability of the text message, as well as its impact on patients initiating HCV discussions with their PCPs. The research staff called participants at a preferred time specified in the initial recruitment call, or two hours after their appointment, if they did not indicate a preference. If participants did not answer this first call, a second call was made within that same day. If this second call was not answered, the research staff left participants a voicemail that provided contact information to return the call. Participants who did not attend their appointments were considered ineligible to complete the post-text message evaluation survey. Regardless of text message type sent, all participants were asked if they talked to their PCP about HCV and then, using an open-ended question, were asked why.
Statistical Analysis
Standard descriptive statistics were used to summarize participant demographics and responses to the post-text message evaluation survey. Participant initiation of HCV discussions between text message groups were compared using a Fisher’s exact test at a 95% confidence interval. Data analysis was conducted with R (version 3.1.2; R Core Team; Vienna, Austria).
Results
Patient Recruitment & Enrollment
A total of 185 patients were called. One hundred nine (59%) answered, of whom 47 (43%) enrolled. Of these 47 participants, 25 (53%) were in the birth cohort. Within the 22 non-birth cohort participants, 18 (82%) were born after 1965, and 4 (18%) were born before 1945. See Figure 1 for all recruitment and enrollment outcomes.
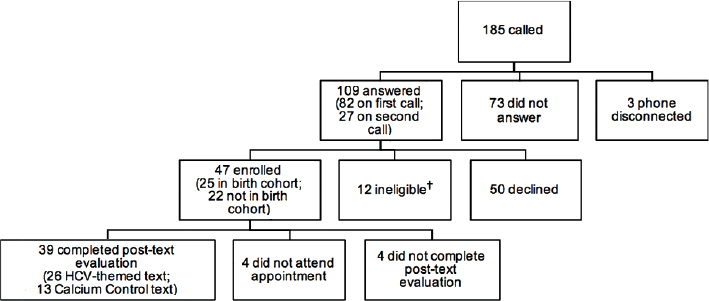
Figure 1: Patient Recruitment and Enrollment.
†Four patients were ineligible because a mutually convenient time for the screening could not be arranged. The other eight ineligible patients were disqualified for the previously stated eligibility criteria.
Post-Text Message Campaign Evaluation
Acceptability of Text Message Campaign
Of the 47 enrolled participants, 39 (83%) completed the post-text message evaluation survey. Of the 34 participants who were sent an HCV-themed text message, 26 (76%) completed the post-text message evaluation survey, while all 13 participants who were sent the calcium control text message completed the post-text message evaluation survey.
Thirty-two (82%) of the 39 participants surveyed liked receiving a health-related text message (88% in the HCV group and 70% in the calcium control group), and 25 (64%) found the message useful (76% in the HCV group and 46% in the calcium control group).
Impact of Text Message Campaign on Participant-PCP HCV Discussions
Of the 39 participants who completed the post-text message evaluation survey, one participant did not read the text message prior to the clinic appointment and was excluded, leaving 38 for analysis. Of these, 25 participants received an HCV-themed text message, and 15 (60%) reported having an HCV-related discussion with their PCP, 10 of whom (40% of all 25) reported initiating this discussion because of the text message. Of the 13 participants who received the calcium control message, none initiated a discussion about HCV with their PCP. Participants who were sent an HCV-themed text message were more likely to initiate discussions with their PCPs about HCV than participants sent the calcium control text message (p=0.008). Of those in the birth cohort, 7 of the 14 (50%) participants who received an HCV-themed text message reported initiating an HCV-related discussion with their PCP because of the text message, while 3 of the 11 (27%) non-birth cohort participants did so. See Figure 2 for overall results of the text message campaign and see Table 2 for results by text message type.
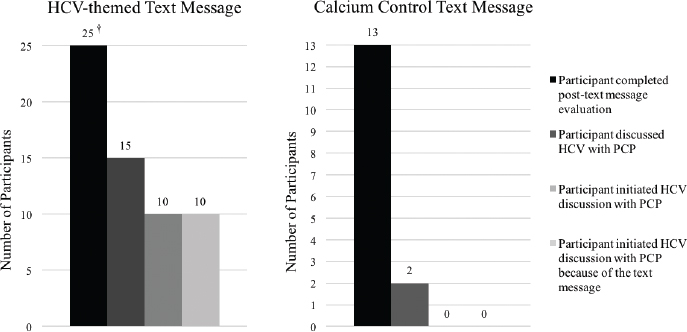
Figure 2: Impact of Text Message Campaign on HCV Discussions.
†Out of 26 participants who received an HCV-themed text message and completed the post-text message evaluation survey, one participant did not read the text message prior to the clinic appointment and was therefore excluded from further analysis; thus, the evaluable number of participants who received an HCV-themed text message was 25.
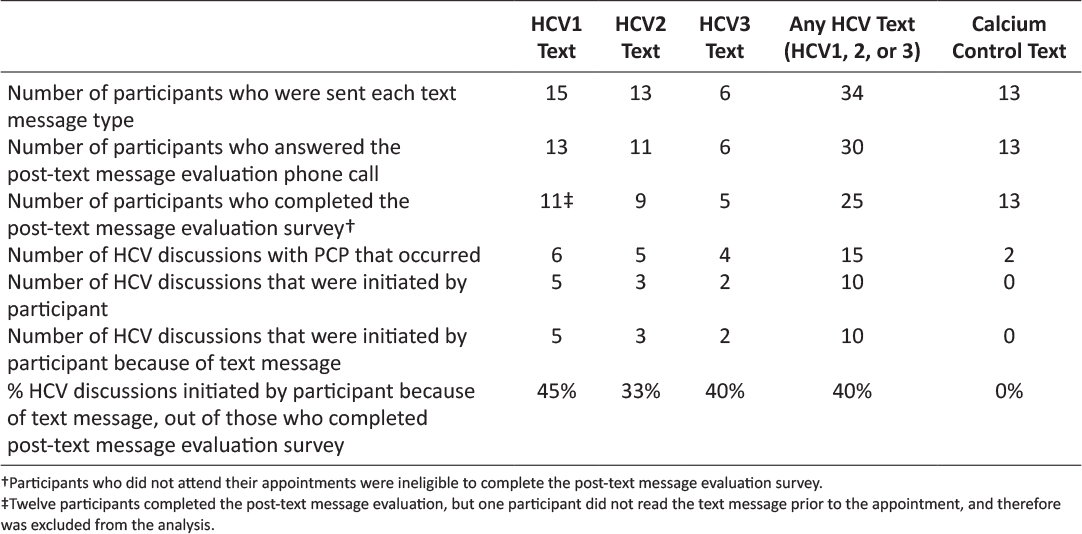
Table 2: Impact of Text Message Campaign on HCV Discussions by Text Message Type.
Discussion
Recruitment Feasibility Outcomes
Our pilot study demonstrated the feasibility of recruiting patients into an HCV text message campaign for the healthcare setting. Using cold call recruitment, nearly 60% of patients answered the phone – an answer prevalence comparable to that achieved in a government-led national survey.21 Once patients answered the phone, nearly half enrolled. This enrollment success may have been because our study required a one-time only intervention and follow-up survey, since time commitment is a critical factor in research study participation.22,23 Also, some patients were pleased to learn of a research partnership between Baylor College of Medicine and their clinic, and patients are more likely to enroll in studies run by persons they trust.24,25 Finally, of those enrolled, over 80% completed all steps of the study. This high retention rate may have resulted from the research staff eliciting participants’ preferred time for the post-text message phone call, implementing flexible strategies that accommodated participants’ needs.26
Acceptability Outcomes
Our HCV text message campaign was found to be acceptable; 82% of participants liked receiving a health-related text message, and, specifically, 88% liked receiving a message with HCV content. As McGuire noted, “liking” a campaign is an “index of persuasive effectiveness.” 27 The formative research that we conducted with members of the target audience to guide HCV text message content likely enhanced our message’s acceptability, as pretesting has been shown to do.28 As for utility, about three-fourths of participants who received an HCV text message found it useful. The messages may have been particularly practical because they addressed previously identified gaps in patient knowledge, such as HCV’s routes of transmission and asymptomatic nature.29
Impact of the HCV Text Message Campaign on Patient-Physician HCV Discussions
This pilot study demonstrated preliminary effectiveness of an HCV text message campaign to empower patients to discuss HCV screening with their physicians. While no participant in the control text message group initiated an HCV discussion with their physician, 40% of participants receiving an HCV text message initiated this discussion. This success could be attributable to several features of our campaign. First, personalization, which is used in most successful text message interventions,30 was a key feature of the text message content. As noted by Hawkins et al., “personalization attempts to increase attention or motivation to process messages by conveying, explicitly or implicitly, that the communication is designed specifically for ‘you.’”31 In our study, each message included the participant’s name and his/her physician’s name, thereby making the message more salient to the receiver. Second, our HCV text message content included a specific cue to action – a key component for stimulating behavior change according to the health belief model.32 Each HCV text message encouraged patients to talk to their physician about HCV screening at the upcoming clinic visit, thereby providing the cue about “when and where” the health action should be done.33 Finally, the messages were delivered at an opportune moment – just before the participant’s appointment – when the health action needed to occur, and optimizing exposure to a campaign’s message is a critical determinant of campaign success.27
Overall, text message campaigns for health promotion and disease prevention have numerous advantages over other types of health-related mass media campaigns. A 2004 review on health communications campaigns reminds campaign planners that messages should be “kept simple, because complicated messages are more likely to be misunderstood and misremembered.”34 Because text messages are limited to 160 characters, messages must be shorter and less complex. Additionally, campaign exposure is a mediator of success that campaign designers struggle to achieve.30,34 However, a text message campaign can be delivered to a specific person at a specific – and even preferred – time, to increase exposure. In the case of text message campaigns for healthcare settings, some electronic medical record (EMR) systems have the capability to send text messages to mobile phones and the advantage of being able to extract personalization and health data (e.g. prior HCV screening results) to deliver relevant and timely messages near clinic visits.
Limitations
There are limitations to our study. This study was conducted in an academic private practice clinic, which serves a socioeconomically advantaged, predominately white patient population. Therefore, our results may not be generalized to other healthcare settings – such as those serving low-income, minority patients, who are often harder to recruit for research and have poorer communication with their physicians.35–37 Additionally, our patient population likely had higher health literacy than racial and ethnic minorities,38 and therefore may have been more comfortable initiating a discussion with a physician.39 Indeed, patients from disadvantaged populations (e.g. lower income, racial/ethnic minorities) are less active in discussions with their physicians,40 and it remains to be seen whether a text message campaign would be equally effective at prompting these patients to have an HCV discussion with their physicians. Finally, while 40% of participants reported discussing HCV screening with their physicians, this result may have been subject to social desirability bias, though the research staff did emphasize to each participant during the post-text message survey that there were no right or wrong answers.
In short, our study was conducted in a relatively homogenous population. Further research is needed to determine the translation of our results to more diverse patient populations. Despite these limitations, this study provides critical proof-of-concept that a patient-facing text message campaign can stimulate HCV discussions in healthcare encounters. Building upon previous work which has shown that minorities are amenable to receiving healthcare reminders, our proof-of-concept study takes the next step towards a larger health campaign focusing on minorities.41
Conclusions
Despite national recommendations for HCV screening,2,3 HCV screening remains suboptimal,4,6 because physicians face barriers to ordering the test, and patients are unaware of their need to be tested.7–10 Our study suggests that a patient-facing HCV screening campaign, based on the push-pull model, could help overcome these barriers. Further research is needed to determine how to optimize recruitment and retention strategies for a health center-based text message campaign study, and a larger study may help confirm our preliminary and promising results. Additionally, the impact of a patient-facing HCV text message campaign on physician orders of HCV tests – the ultimate metric of an HCV screening campaign’s success – needs to be determined.
Acknowledgments
The authors would like to thank Anna Kimutis for her work in developing the text message content and data collection instrument, as well as in implementing the early study design. The authors also want to thank Kira Chen, Cierra Duckworth, Edna Otuomagie, and Michelle Won for their assistance in developing the text message content, as well as Dr. Kirsten Ostherr for her collaboration. Finally, the authors would like to thank Disha Kumar for her thoughtful review of the final manuscript draft.
Conflict of Interest Statement
None of the authors have a conflict of interest or funding source related to this work to report. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs or the United States government.
Financial Disclosure
The authors have financial disclosures, including: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This research was supported in part by the Center for Innovations in Quality, Effectiveness and Safety, Michael E. DeBakey VA Medical Center. Dr. Murphy is additionally funded by an Agency for Healthcare Research & Quality Mentored Career Development Award (K08-HS022901).
References
1. Centers for Disease Control and Prevention. Hepatitis C FAQs for Health Professionals [Internet]. Centers for Disease Control and Prevention. 2017 [cited 2017 Aug 14]. Available from: https://www.cdc.gov/hepatitis/hcv/hcvfaq.htm#a5
2. Centers for Disease Control and Prevention. Testing Recommendations for Hepatitis C Virus Infection [Internet]. Centers for Disease Control and Prevention. 2015 [cited 2017 Aug 15]. Available from: https://www.cdc.gov/hepatitis/hcv/guidelinesc.htm
3. Moyer VA. Screening for Hepatitis C Virus Infection in Adults: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2013 Sep 3;159(5):349–57. ![]()
4. Centers for Disease Control and Prevention. Recommendations for the Identification of Chronic Hepatitis C Virus Infection Among Persons Born During 1945–1965 [Internet]. Centers for Disease Control and Prevention; 2012 Aug [cited 2017 Aug 15] p. 4. (Morbidity and Mortality Weekly Report). Report No.: 4. Available from: https://www.cdc.gov/mmwr/pdf/rr/rr6104.pdf
5. Centers for Disease Control and Prevention. People Born 1945-1965 & Hepatitis C [Internet]. Centers for Disease Control and Prevention. 2015 [cited 2017 Aug 15]. Available from: https://www.cdc.gov/hepatitis/populations/1945-1965.htm
6. Jemal A, Fedewa S. Recent Hepatitis C Virus Testing Patterns Among Baby Boomers. Am J Prev Med. 2017 Jul;53(1):e31–3. ![]()
7. Thomson M, Konerman MA, Choxi H, Lok ASF. Primary Care Physician Perspectives on Hepatitis C Management in the Era of Direct-Acting Antiviral Therapy. Dig Dis Sci. 2016 Dec 1;61(12):3460–8. ![]()
8. Clark E, Yawn B, Galliher J, Temte J, Hickner J. Hepatitis C Identification and Management by Family Physicians. Fam Med. 2005 Oct;37(9):644–9.
9. Falade-Nwulia O, McAdams-Mahmoud A, Irvin R, Niculescu A, Page KR, Mix M, et al. Primary Care Providers Knowledge, Attitude and Practices Related to Hepatitis C Screening and Treatment in the Oral Direct Acting Antiviral Agents Era. J Community Med Health Educ. 2016 Oct 28;1–6. ![]()
10. Jewett A, Garg A, Meyer K, Wagner LD, Krauskopf K, Brown KA, et al. Hepatitis C Virus Testing Perspectives Among Primary Care Physicians in Four Large Primary Care Settings. Health Promot Pract. 2015 Mar 1;16(2):256–63. ![]()
11. Coppola AG, Karakousis PC, Metz DC, Go MF, Mhokashi M, Howden CW, et al. Hepatitis C Knowledge among Primary Care Residents: Is Our Teaching Adequate for the Times? Am J Gastroenterol. 2004 Sep;99(9):1720. ![]()
12. Pew Research Center. Mobile Fact Sheet [Internet]. Pew Research Center: Internet, Science & Tech. 2017 [cited 2017 Aug 15]. Available from: http://www.pewinternet.org/fact-sheet/mobile/
13. Smith A. Americans and Text Messaging [Internet]. Pew Research Center; 2011 Sep [cited 2017 Aug 15] p. 1–14. Available from: http://www.pewinternet.org/2011/09/19/americans-and-text-messaging/
14. Smith A. U.S. Smartphone Use in 2015 [Internet]. Pew Research Center: Internet, Science & Tech. 2015 [cited 2017 Aug 15]. Available from: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/
15. Martin LR, DiMatteo MR. The Oxford Handbook of Health Communication, Behavior Change, and Treatment Adherence. OUP USA; 2013. 537 p. ![]()
16. Cole-Lewis H, Kershaw T. Text Messaging as a Tool for Behavior Change in Disease Prevention and Management. Epidemiol Rev. 2010 Apr;32(1):56–69. ![]()
17. Patel S, Hemmige V, Street, Jr. R, Viswanath K, Arya M. Activating Racial and Ethnic Minorities to Engage in Preventive Health: Patient Preferences for Health Reminders. J Particip Med [Internet]. 2017 Apr 22; Available from: https://participatorymedicine.org/journal/evidence/research/2017/04/22/activating-racial-and-ethnic-minorities-to-engage-in-preventive-health-patient-preferences-for-health-reminders/
18. Zallman L, Bearse A, West C, Bor D, McCormick D. Patient Preferences and Access to Text Messaging for Health Care Reminders in a Safety-net Setting. Inform Health Soc Care. 2017 Jan 2;42(1):32–42. ![]()
19. Levine J, Cohen S, Harkin P, Guydish J, Sorensen J, Masson C. Acceptability of a Mobile Phone Based Hepatitis C Intervention. Drug Alcohol Depend. 2015 Nov 1;156:e127. ![]()
20. Arya M, Kumar D, Patel S, Street RL, Giordano TP, Viswanath K. Mitigating HIV Health Disparities: The Promise of Mobile Health for a Patient-Initiated Solution. Am J Public Health. 2014 Dec;104(12):2251–5. ![]()
21. Ahmed WM, Kalsbeek WD. An Analysis of telephone call history data from the behavioral risk factor surveillance system. In: Proceedings of the Survey Research Station. American Statistical Association; 1998. p. 224–9.
22. Kurt A, Kincaid HM, Curtis C, Semler L, Meyers M, Johnson M, et al. Factors Influencing Participation in Clinical Trials: Emergency Medicine vs. Other Specialties. West J Emerg Med. 2017 Aug;18(5):846–55. ![]()
23. Swanson GM, Ward AJ. Recruiting minorities into clinical trials: toward a participant-friendly system. J Natl Cancer Inst. 1995 Dec 6;87(23):1747–59. ![]()
24. Public Perception of Clinical Trials [Internet]. Research!America; 2017 Jul. Available from: http://www.researchamerica.org/sites/default/files/July2017ClinicalResearchSurveyPressReleaseDeck_0.pdf
25. McDonald AM, Treweek S, Shakur H, Free C, Knight R, Speed C, et al. Using a business model approach and marketing techniques for recruitment to clinical trials. Trials. 2011 Mar 11;12:74. ![]()
26. Clinical Trials Recruitment Best Practices Manual [Internet]. Michael J. Fox Foundation for Parkinson’s Research; 2011 Mar. Available from: https://www.michaeljfox.org/files/MJFF_Recruitment_Best_Practices_manual.pdf
27. McGuire W. McGuire’s Classic Input-Output Framework for Constructing Persuasive Messages. In: Public Communication Campaigns. 4th ed. Thousand Oaks, CA: SAGE Publications, Inc; 2012. p. 392.
28. National Cancer Institute (U S.) Office of Communications. Making Health Communication Programs Work: A Planner’s Guide. United States Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 2004. 251 p.
29. Calderon Y, Cowan E, Schramm C, Stern S, Brusalis C, Iscoe M, et al. HCV and HBV testing acceptability and knowledge among urban emergency department patients and pharmacy clients. Prev Med. 2014 Apr;61:29–33. ![]()
30. Head KJ, Noar SM, Iannarino NT, Grant Harrington N. Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Soc Sci Med. 2013 Nov 1;97(Supplement C):41–8. ![]()
31. Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Educ Res. 2008 Jun;23(3):454–66. ![]()
32. Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver J. The Health Belief Model as an Explanatory Framework in Communication Research: Exploring Parallel, Serial, and Moderated Mediation. Health Commun. 2015;30(6):566–76. ![]()
33. Silk K, Atkin CK, Salmon C. Developing effective media campaigns for health promotion. In: Handbook of health communication. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 2011. p. 203–19.
34. Snyder LB. Health communication campaigns and their impact on behavior. J Nutr Educ Behav. 2007 Apr;39(2 Suppl):S32-40. ![]()
35. Gorelick PB, Harris Y, Burnett B, Bonecutter FJ. The recruitment triangle: reasons why African Americans enroll, refuse to enroll, or voluntarily withdraw from a clinical trial. An interim report from the African-American Antiplatelet Stroke Prevention Study (AAASPS). J Natl Med Assoc. 1998 Mar;90(3):141–5.
36. Ford JG, Howerton MW, Lai GY, Gary TL, Bolen S, Gibbons MC, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: A systematic review. Cancer. 2008 Jan 15;112(2):228–42. ![]()
37. Gordon HS, Street RL, Sharf BF, Souchek J. Racial differences in doctors’ information-giving and patients’ participation. Cancer. 2006 Sep 15;107(6):1313–20. ![]()
38. National Center for Educational Statistics. National Assessment of Adult Literacy (NAAL): A First Look at the Literacy of America’s Adults in the 21st Century. Washington, DC: Institute of Education Sciences, US Department of Education; 2005.
39. Aboumatar HJ, Carson KA, Beach MC, Roter DL, Cooper LA. The impact of health literacy on desire for participation in healthcare, medical visit communication, and patient reported outcomes among patients with hypertension. J Gen Intern Med. 2013 Nov;28(11):1469–76. ![]()
40. Street RLJ, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient Participation in Medical Consultations: Why Some Patients are More Involved Than Others. Med Care. 2005 Oct;43(10):960. ![]()
41. Patel S, Hemmige V, Street RL, Viswanath K, Arya M. Activating Racial and Ethnic Minorities to Engage in Preventive Health: Patient Preferences for Health Reminders. J Particip Med [Internet]. 2017 [cited 2018 Sep 15];9. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5736376/

