Use of Personal Devices in Healthcare: Guidelines From A Roundtable Discussion
Use of Personal Devices in Healthcare: Guidelines From A Roundtable Discussion
Laura Vearrier, MD1, Kyle Rosenberger, M.Ed2, Valerie Weber, DMD, MA3
1Assistant clinical professor, Department of Emergency Medicine, Drexel University College of Medicine, Philadelphia, PA; 2Instructional Designer, Ohio University Heritage College of Osteopathic Medicine and Ohio University’s Office of Instructional Innovation, Athens, OH; 3Assistant clinical professor, Department of General Dentistry and Oral Medicine, University of Louisville School of Dentistry, Louisville, KY.
Note: The corresponding author is not a recipient of a research scholarship.
Journal MTM 7:2:27–34, 2018
Background: In recent years, smartphone use in professional settings has been increasing, particularly with physicians. There are benefits and drawbacks that result from this increase. Despite this, there is relatively limited peer-reviewed medical literature on the subject. Thus, suitable guidelines for smartphone use in the health care setting is needed.
Aims: This article present guidelines for professional conduct related to the use of personal devices, such as smartphones, in the healthcare setting.
Methods: These guidelines were developed through an interdisciplinary roundtable discussion at the 2016 Academy for Professionalism in Health Care Conference in Philadelphia, PA.
Results: As a result of the roundtable discussions, several guidelines were developed. First, healthcare providers should be trained on the danger of distractions caused by personal devices and how to minimize them in a clinical setting. Second, the use of smartphones for personal use should be limited to specified use areas; however, if they are present during a patient encounter, they should be set to a mode that eliminates or minimizes interruptions. Third, providers should seek permission from patients prior to integrating smartphones into the provider-patient relationship. Finally, smartphone photography, while being a potential tool to improve patient care, should be used with caution concerning patient autonomy and privacy.
Conclusion: The guidelines serve as a foundation from which professionalism with regard to personal device use can be further developed.
Keywords: Professionalism, Smartphone, Physicians, Photography, Delivery of Health Care, Clinical Practice, Telemedicine
Introduction
In the last few years, the use of personal devices such as smartphones has been rapidly increasing and smartphone ownership is highest among young adults of higher income and education level.1–2 This trend is being mirrored in the healthcare setting. Nearly all physicians and nurses own smartphones.3–4 Physicians’ usage of smartphones for professional purposes has been steadily increasing from 68% in 2012 to 84% in 2015.5 The Boston Consulting Group and Telenor Group remarked that the “smartphone is the most popular technology among doctors since the stethoscope”.6 A survey study of nurses reported that more than half of nurses have used their smartphone instead of asking a colleague for information.4
There are benefits and drawbacks of providers utilizing their smartphones in the healthcare setting for personal and professional purposes. With computing power and Internet connectivity, personal devices give providers access to textbooks, journal articles, practice guidelines, clinical calculators, and medical applications. Smartphones are improving the efficiency and accuracy of communication. Physicians and nurses are using short messaging services (SMS) to communicate patient information and smartphones have been reported to increase the connectedness of medical trainees’ with their supervisors.7–9 Smartphones are also improving communication between providers and patients. The use of videos on personal devices has been reported to be an efficient and effective way to educate patients on their disease that resulted in increased medication compliance and physicians are using smartphones to monitor patients remotely.10,11 Drawbacks of such constant connectivity include a risk for distraction from patient care. Providers may be interrupted for less acute clinical issues in addition to personal calls, texts, emails, social media, and applications. Personal devices also create a physical barrier between the user and the rest of the world. This barrier translates into cognitive and psychological barriers, and patients are often unaware of the clinical benefits of smartphones.12,13
Despite the ubiquity of smartphones in healthcare, there is limited peer-reviewed medical literature on issues with respect to the professionalism of smartphone use in the healthcare setting. An Ovid Medline keyword search of “professionalism” and the intersection of any of the following: “smartphone”, “smart phone”, “cell phone”, “mobile phone”, “tablet” or “personal device”, yielded only seven results (search performed May, 2016). There is a need for guidance and education regarding professional conduct and personal device use in the healthcare setting. In a survey study of medical students, the majority reported insufficient education from either their medical school curriculum or their senior residents or attendings on appropriate/inappropriate use of mobile devices to communicate patient information and how to conduct themselves professionally with mobile technology.14
Methods
A roundtable workshop exploring issues of professionalism and smartphone use in the healthcare setting was held at The Academy for Professionalism in Health Care 2016 conference in Philadelphia, PA. Participants included physicians, nurses, medical students, dentists and academic researchers. Participant occupational settings included medical education, academic clinical practice, and private practice. Four case-based scenarios (Figure 1) were discussed in small focus groups and then presented to the entire workshop for further analysis. The results of these discussions were compiled into the following guidelines.
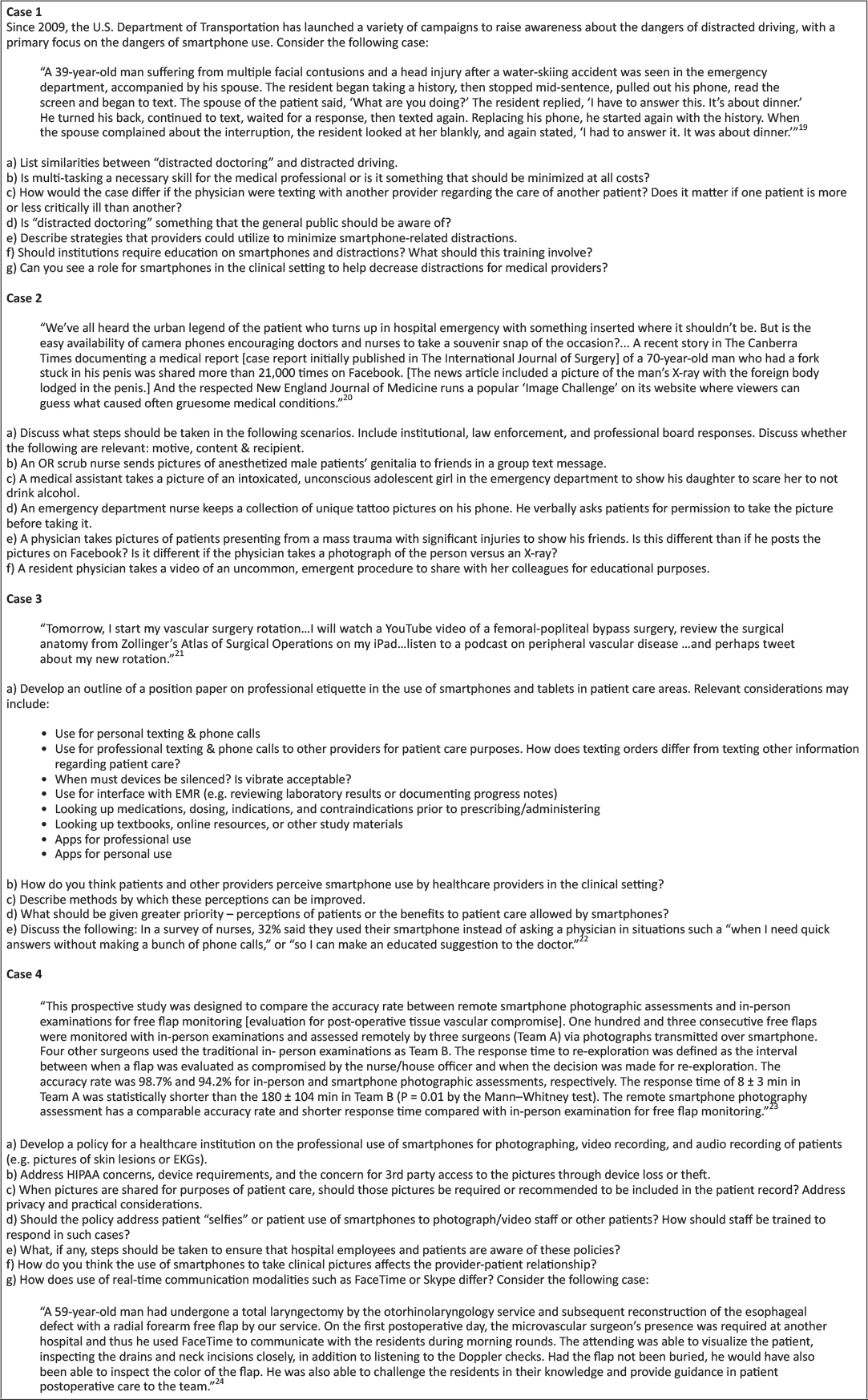
Figure 1: Case-based scenarios and questions
Results
Distraction and Smartphone Use
Smartphone use may result in provider distraction or so-called “distracted doctoring” and increase the risk for patient care errors. Smartphone use in the healthcare setting has the potential to result in distraction in a manner similar to driving. Use of smartphones may involve cognitive, visual, and/or manual tasks that divert the provider’s attention from their patient care responsibilities. As such, frequently repeated activities or procedures may increase the risk that providers will engage in distracting secondary tasks, such as smartphone use. “Bring Your Own Device” (BYOD) policies that require providers to utilize their personal devices for professional purposes may increase the risk of distraction due to non-professional phone calls, text messages, and app notifications. Further research is needed in the area of distracted doctoring and smartphone use.
Healthcare providers commonly hold the misperception that utilizing smartphones for multi-tasking in the healthcare setting improves efficiency and patient care. Professional and personal smartphone utilization in the healthcare setting increases the number of interruptions and the amount of information received and processed by providers while engaging in patient care. While multi-tasking is a necessary skill, it should be minimized when possible. Attentional shifts while multi-tasking interrupt the cognitive processing of information, situational awareness, and may increase the likelihood of patient care errors. Interruptions may be minimized by use of “silent”, “airplane”, and “do not disturb” modes, particularly during important patient care activities. The amount of information received by providers may be controlled through specialized ring or text message tones and disabling of app notifications.
Healthcare providers should be educated on the dangers of “distracted doctoring”. Individuals may overestimate their ability to engage in smartphone use without significant distraction. Education on distraction, generally, and specifically smartphone-associated distraction should be implemented at the undergraduate and graduate medical education levels and in patient-safety-related continuing education. Simulation exercises allow participants to experience the detrimental effects of distraction and develop skills for dynamic prioritization of incoming information.
Appropriate smartphone use may decrease distractions and should be encouraged. Smartphones may be utilized to reduce distractions from handheld pagers and overhead paging systems. Use of calendar functions, alarms, and notes apps may be used to reduce the cognitive load of “to-do lists”. Alarms for medication administration or other time-sensitive tasks may improve timeliness of administration. Smartphone information resources and clinical calculators reduce the need to interrupt current tasks to find a computer. Policies to utilize smartphones to reduce distractions should be considered at the institutional level.
Smartphone Photography in the Healthcare Setting
Smartphone photography is an advantageous learning and communication tool; however, respect for the patient and the patient’s privacy must be paramount. Smartphone photography has the potential to capture disease conditions and procedures that may otherwise be difficult or impossible to record and which may be used in educational materials or the peer-reviewed literature and therefore improve patient care on a global level. Smartphone photography may be used to transfer information about patients (e.g. lesion, electrocardiogram) to other providers, improving the clinical decision-making process and therefore improve patient care on the individual level. Pitfalls of photography in the healthcare setting include capture of patients while they are vulnerable or when they are unable to fully consent. Patients may perceive an element of coercion when asked to be photographed even if no direct coercive statement is made. The individual right to privacy, respect, and autonomy are paramount. Respect for privacy and autonomy as it pertains to smartphone photography should be taught at the undergraduate, graduate and continuing education levels. When institutional photography equipment is available, that equipment should be used in lieu of a smartphone.
Consent should be obtained at the time of image capture for the photograph, the intended use and any transmission. Consent should not be obtained at time of admission or triage for later photography. Consent for photography at that time contains an element of implied coercion and is too abstract to be considered informed consent. Informed consent should include the elements of the body part to be photographed, the intended use, and any transmission of the photograph. When possible, written consent should be obtained. If written consent is not possible, verbal consent should be witnessed and documented.
Photographs should be obtained in such a way as to minimize or eliminate the amount of protected health information that is captured. Photographs of the face are typically not necessary. Patient identifiers such as name, date of birth, and medical record numbers should not be included in photographs. Tattoos, piercings, skin conditions, and other unique identifiers compromise patient confidentiality and should be included only with explicit consent and when capture of those elements is required.
Smartphone photography in the healthcare setting for personal or entertainment purposes is inappropriate and should be avoided. Such photography contains too much potential for abuse to be acceptable. Unintended consequences include the inadvertent capture of protected health information or other patient identifiers. The content of seemingly innocuous photographs in the healthcare setting have the potential to distress patients, family members and others.
Healthcare providers have a duty to intervene in situations involving inappropriate smartphone photography. When possible, inappropriate photography should be prevented. If such photography has already occurred, appropriate interventions may include education, deletion of the photograph, or report at the institutional or law enforcement level depending on the scenario. Healthcare institutions should have protocols in place for reporting inappropriate smartphone photography with a well-defined chain of command and protections against retribution including the ability to anonymously report. Patients may similarly take inappropriate smartphone photographs in the healthcare setting and providers should intervene in those situations as well.
Smartphone etiquette and perceptions
Use of smartphones for personal calls, texting and social media apps is to be avoided in patient care areas. Personal use of smartphones in patient care areas may convey an informality or lack or professionalism to patients, their families, and other staff. Even when providers are not actively engaged in patient care activities, personal smartphone use should be avoided. Patients may perceive that aspects of their care are being adversely affected by personal smartphone use such as wait time, face time with providers, or attention to their complaints. Personal smartphone use may be permitted in staff lounge areas, provided that it does not adversely affect patient care.
Smartphones should be set to “silent”, “airplane”, or “do not disturb” modes during patient encounters. Vibrate modes are frequently audible and should not be utilized. App notifications should be turned off using one of the above-mentioned modes. Smartphone interruptions during sensitive discussions may be particularly distressing to patients. It is encouraged to remind colleagues to put their smartphone into one of the above-mentioned modes prior to such a discussion. Most healthcare providers do not need to be immediately available to colleagues. In the event that a healthcare provider must be immediately available during a patient encounter, the possibility of interruption should be communicated to the patient at the outset. The use of a “do not disturb” mode that permits calls from only pre-identified emergency contacts may reduce the risk of interruption and is recommended.
Patient permission should be obtained for professional smartphone utilization during patient care activities. As discussed above, smartphones are a resource for healthcare professionals, allowing increased communication with other providers, interface with EMR, clinical calculators, and immediate access to information resources (e.g. pharmacopeia). The inherent portability of smartphones over other electronic devices makes them particularly useful during patient care activities. However, explicit patient permission should be obtained prior to their utilization during patient care activities. Permission introduces the device into the patient-provider relationship and serves the dual purpose of informing the patient that the device is being used to facilitate their care and to confirm that use of the device will not be unduly distressing to the patient. Patients should be encouraged to ask their physicians what they are using their devices for to facilitate communication regarding this practice.
Transparency during professional smartphone use minimizes negative patient perceptions associated with provider smartphone utilization and is encouraged. Patients should be informed of the specific tasks being performed by the provider that are facilitating their care. When smartphones are being used to access EMR, clinical calculators, and information resources, sharing the smartphone screen with the patient provides transparency and empowers the patient to participate in their care. Visual information shared by smartphone device augments the verbal exchange of information between patient and provider and facilitates shared decision making.
Institutional policies on smartphone use
Institutions should have policies delineating appropriate and inappropriate smartphone use and notify employees of these policies. Considerations in the development of such policies must include patient care versus non-patient care areas, the rights of employees, patient safety and privacy, and professional versus personal use. Disciplinary actions may range from verbal warnings with documentation to dismissal depending on the offense. Administration should develop smartphone photography policies and outline the consequences for misuse. Institutional policies should also address smartphone use by patients and their families.
When personal smartphones are utilized for patient care activities, institutional policy should address device encryption and password protection. Institutions have a duty to patients and providers to reasonably protect their privacy against breaches. Difficulties associated with institutional oversight of personal devices may require that efforts are directed at provider education and institution-provider contracts on device parameters and use. Mandatory reporting of lost devices and remote wiping capabilities are appropriate policies. Multi-factor authentication should be considered for access to protected health information. Long-term storage of patient-related data or photographs on a personal device is inappropriate. While not all breaches in confidentiality are preventable, reasonable institutional oversight minimizes the risk and ramifications of such a breach.
When smartphone photography is used for patient care, the images should be integrated into the medical record. Institutions should have a mechanism by which smartphone photographs may be readily incorporated into the paper or electronic medical record and provide education to providers in this regard. Requiring integration into the medical record at the time that patient care is delivered minimizes the length of time that the image is retained on a personal device and risk that the provider fails to upload the photograph to the medical record.
Policies delineating the appropriateness of smartphones for telemedicine are encouraged. Such policies should be in accordance with state and federal laws. Video and conferencing apps enable remote care of patients and interdisciplinary cooperation, which enhance patient care when utilized appropriately. Telemedicine is not a replacement for bedside patient care when such care is reasonably available.
Discussion
Professional and non-professional uses of smartphones can create distractions that can be detrimental to patient care. Healthcare providers should be educated on the dangers of distractions and be trained on how to minimize distractions related to personal devices. The use of smartphone functions, such as alarms, notes, and direct inter-provider communications, to decrease distraction is encouraged. Further research is needed in the area of distracted doctoring to determine the scope of this problem and the most effective intervention strategies.
Smartphone photography has the potential to improve patient care on the global and individual level but is associated with many pitfalls due to the ease and ubiquity of smartphone photography in general. Patient autonomy and privacy are paramount. Respect for the patient always trumps any potential benefit, global or individual, afforded by a photograph. Consent should be obtained just prior to obtaining a photograph and should be witnessed and documented. Photographs or videos for entertainment or personal uses is not appropriate. Providers have a duty to peer-regulate and intervene in the case of inappropriate smartphone use. Healthcare institutions should have protocols for reporting and addressing inappropriate use of smartphone photography.
The use of smartphones for personal applications should be limited to designated break or lounge areas. Smartphones should be set to modes that eliminate or minimize interruptions during patient encounters. Providers should seek permission from patients prior to integrating smartphones into the provider-patient relationship to improve communication and education. Providers should strive for transparency with regard to their professional use of smartphones explain and show to patients the clinical applications of smartphones.
These guidelines do not address legal aspects of restricting mobile phone use in clinical settings; however, they serve as a basis for the conversation to begin. While the Medicines and Healthcare Products Regulatory Agency (MHRA) does not support a blanket ban on the use of mobile phones in hospitals, some health systems are taking it upon themselves to implement regulations.15 For example, the Jewish General Hospital in Montreal, Quebec, has instituted a policy that addresses “the use of cell phones in the hospital for phone calls and for data usage (including text messages, browsing the internet or other). This policy applies to all cell phone users in the hospital, including staff, members of the CPDP, consultants, volunteers, visitors, and patients.”16 This policy looks to mitigate the use of mobile devices to respect the patients’ rights, with a focus on safety and confidentiality. Another hospital, Union Hospital in Eklton, Maryland, has issued a policy that includes advising employees that the “use of cell/camera phone during work, for other than hospital business should be avoided. Personal calls should be limited to break and meal breaks. All employees are required to silence their cell/camera phones while they are working.”17 Similarly, Greenville Hospital System in Greenville, South Carolina does not look to outright band mobile phone use, but advises that,
“During work time, employees are expected to exercise the same discretion with the use of personal communication devices as is expected with the use of any business phone. Personal phone calls (including text messaging) during the work day, regardless of the phone or device used, are not appropriate can interfere with productivity and be distracting to others.”18
While these are only a few examples of hospitals and health systems that have instituted policies around mobile devices, they do demonstrate a growing movement towards regulating such devices. This movement, while presumably controversial, is a natural occurrence as the prevalence of mobile technology increases. As such, hospitals and health systems will need to take a position on how strict their regulations will be, with the goal of improving patient care and safety.
Conclusion
As personal devices are becoming a technology that is integral to patient care, healthcare institutions should develop written policies regarding smartphone use. Policies should address appropriate use, consequences of misuse, mechanisms to protect patient information, integration of communication and images into medical records, and guidelines for telemedicine.
These guidelines establish a foundation for the professional use of smartphones in the healthcare setting. The very nature of smartphones, as personal devices, mandates that the use of smartphones be largely regulated on the individual and peer level. This self-regulation demands a strong internal locus of professionalism that must be developed, practiced, and assessed among all healthcare professionals.
Acknowledgements
The authors wish to acknowledge Nicholas DeVito, MPH; Lucy Hammond, PhD; Marguerite Heyns; Mark Kuczewski, PhD; Dennis Novack, MD; Steven Rosenzweig, MD; and Glen Solomon, MD for their significant contributions to the roundtable discussions.
References
1. Pew Research Center. Technology Device Ownership: 2015 [Internet]. 2015. [cited 23 January 2017]. Available from: http://www.pewinternet.org/2015/10/29/technology-device-ownership-2015/pi_2015-10-29_device-ownership_0-01/.
2. Anderson M. 6 facts about Americans and their smartphones [Internet]. 2015. [cited 23 January 2017] Avialable from: http://www.pewresearch.org/fact-tank/2015/04/01/6-facts-about-americans-and-their-smartphones/.
3. Wiechmann W, Kwan D, Bokarius A, et al. There’s an App for That? Highlighting the Difficulty in Finding Clinically Relevant Smartphone Applications. West J Emerg Med. 2016;17:2:191–4. ![]()
4. Kern C. Nurses Use Smartphones, Apps More Than Doctors. [Internet]. 2015 [cited 23 January 2017]. Available from: http://www.healthitoutcomes.com/doc/nurses-use-smartphones-apps-more-doctors-0001.
5. Statista. Physicians’ usage of smartphones for professional purposes in the U.S. from 2012 to 2015. [Internet]. 2015. [cited 23 January 2017]. Available from: http://www.statista.com/statistics/416951/smartphone-use-for-professional-purposes-among-us-physicians/.
6. Telenor Group. New study: The world is ready for mobile healthcare. [Internet]. 2012. [cited 23 Janaury 2017]. Available from: https://www.telenor.com/media/press-releases/2012/new-study-the-world-is-ready-for-mobile-healthcare/.
7. Prochaska M, Bird A, Chadaga A, Arora V. Resident Use of Text Messaging for Patient Care: Ease of Use or Breach of Privacy?. J Med Internet Res. 2015; 3(4):e37.
8. McCartney P. Texting protected health information in healthcare. MCN. Am J Matern Child Nurs. 2015; 40(1):61. ![]()
9. Wu R, Tzanetos K, Morra D, Quan S, Lo V, Wong B. Educational impact of using smartphones for clinical communication on general medicine: More global, less local. J Hosp Med. 2013; (7):365. ![]()
10. T, Smith S. Using digital videos displayed on personal digital assistants (PDAs) to enhance patient education in clinical settings. Int J Med Inform 2007;76:829–35. ![]()
11. Lei W, Pedersen P, Strong D, Tulu B, Agu E, Ignotz R. Smartphone-based wound assessment system for patients with diabetes. IEE Biomed Health Inform. 2015; (2): 477.
12. Miller K, Ziegler C, Greenberg R, Patel P, Carter M. Why Physicians Should Share PDA/Smartphone Findings With Their Patients: A Brief Report. J Health Commun. 2012;17:54–61. ![]()
13. Hsieh C, Yun D, Bhatia A, et al. Patient perception on the usage of smartphones for medical photography and for reference in dermatology. Dermatol Surg. 2015;41 (1):149–54. ![]()
14. Tran K, Lo V, Abrams H, Wu R, Morra D, Quan S. Medical students and personal smartphones in the clinical environment: The impact on confidentiality of personal health information and professionalism. J Med Internet Res. 2014;16(5): e132. ![]()
15. Muhammed R. Banning mobile phones in hospitals: is there enough evidence? Arch Dis Child. 2006;91(12):1043.
16. Jewish General Hospital. A new policy regulates the use of cell phones in hospital facilities, taking into consideration technical, ethical and practical issues [Internet]. n.d. [cited 2018 May 9]. Available from: http://jgh.ca/uploads/common/jgh%20cell%20 phone%20policy.pdf.
17. Union Hospital. Hospital policies and procedures: cell/camera phone use [Internet]. 2015 [updated 2015 Feb; cited 2018 May 9]. Available from: https://www.uhcc.com/wp-content/uploads/2016/03/HR-325-Cell-Camera-Phone-Policy.pdf.
18. Greenville Hospital System. Manual of policy directives: use of cell phones and other portable communication devices [Internet]. 2010 [cited 2018 May 9]. Available from: http://hsc.ghs.org/wp-content/uploads/2013/12/Use-of-Cell-Phones-and-Other-Portable-Communication-Devices.pdf.
19. Ross S, Forgie S. Distracted doctoring: smartphones before patients?. CMAJ [serial on the Internet]. (2012, Sep 4), [cited 29 January, 2017];184(12): 1440.
20. Corderoy A. Smartphones raise privacy issues in healthcare. Sydney Morning Herald. [Internet]. 2013. [cited 29 January 2017] Available from: http://www.smh.com.au/digital-life/digital-life-news/smartphones-raise-privacy-issue-in-healthcare-20130912-2tm51.html#ixzz45j4Btzqh.
21. Farooq A, White J. #Nomoretextbooks? The impact of rapid communications technologies on medical education. Can. J. Surg [serial on the Internet]. (2014, Jan 1), [cited 29 January 2017]; 57(4): E119-E120.
22. Miliard M. Nurses turning to smartphones for clinical advice. Healthcare IT News. [Internet]. 2015. [cited 29, January 2017] Available from: http://www.healthcareitnews.com/news/nurses-turning-smartphones-clinical-advice.
23. Engel H, Huang J, Tsao C, Lin C, Chou P, Cheng M, et al. Remote real-time monitoring of free flaps via smartphone photography and 3G wireless internet: A prospective study evidencing diagnostic accuracy. Microsurgery [serial on the Internet]. (2011, Nov), [cited 29 January 2017];31(8): 589.
24. Kaltman J, Best S, Kaltman S. Virtual rounding via videoconference-enabled smartphones: A case for multifacility rounds. Oral Surg Oral Med Oral Pathol Oral Radiol Endod [serial on the Internet]. (2012, June 1), [cited 29 January 2017];113(6): e15–e18.

