Finding Time for Sleep: Identifying Sleep Concerns in Non-Sleep Specialty Clinics using the MySleepScript App
Finding Time for Sleep: Identifying Sleep Concerns in Non-Sleep Specialty Clinics using the MySleepScript App
Ankur Doshi, BA1, Charlene E. Gamaldo, MD1, Peter Dziedzic, MS1, Alyssa Gamaldo, PhD2, Anthony Kwan, BA1, Luis Buenaver, PhD1, Seulah Choi, BS1, Annette Wang, BS1, Aadi Kalloo, BA1, Rachel E. Salas, MD1
1Johns Hopkins University School of Medicine, Baltimore, MD; 2School of Aging Studies, University of South Florida, Tampa, FL
Author Information: Rachel Salas, MD 600 N. Wolfe Street Baltimore, MD 21287 443 287 0422.
Corresponding Author: rsalas3@jhmi.edu
Journal MTM 6:2:19–27, 2017
Background/Aims: To determine the utility and feasibility of implementing an mhealth tool into the clinical workflow of non-sleep specialists to assist in the evaluation, management, and education of patients with disrupted sleep.
Methods: MySleepScript is a clinical iPad® App developed by an interdisciplinary team of sleep experts that allow healthcare providers to screen and educate their patients who demonstrate symptoms concerning for unhealthy sleep behaviors and sleep-related difficulties. MySleepScript was conducted in 5 outpatient specialty clinics from 07/2014-9/2015. Patients were asked to answer questions regarding sleep habits, behaviors, and environment. Based on the patient responses, providers were provided a report regarding the “level of concern” for potential sleep disorders as well as customized sleep educational information for their patients. Patients were asked to complete satisfaction surveys.
Results: Of 120 patients, 66% completed the app within 15 minutes (87% within 20). Positive results were collapsed (strongly agree or agree). Ninety-four percent of patients found the app easy to use, 78% preferred the app platform to paper, 83% felt it enhanced communication with provider, 65% found the educational output helpful. Ninety-one percent recommend providers continue using MySleepScript. No significant differences across participant characteristics were observed for satisfaction survey responses regarding ease of use, preference over paper, or recommendation to continue using app. Degree of enthusiasm for MySleepScript was particularly high among non-Caucasian patients.
Conclusions: Our results demonstrate the feasibility of an mhealth sleep clinical tool conducted across a diverse patient population with uniform demonstration of increased overall patient satisfaction.
Introduction
Millions of Americans currently suffer with disrupted sleep, many of whom with undiagnosed and untreated sleep disorders.1 Sleep disturbances and disorders are a public health epidemic resulting in roughly 16 billion dollars in direct medical costs annually and 150 billion dollars in reduced workplace productivity in the United States alone.2,3 Poor sleep can negatively impact cognitive performance,4 mood,5 metabolism,6 quality of life,7,8 and life expectancy.1,8 Disrupted sleep is also significantly associated with several chronic conditions, including but not limited to diabetes mellitus,8,9 hypertension,6 cardiac disease,6,7 psychiatric disorders,1 obesity,9 and chronic pulmonary disease.8,10 Furthermore, sleep disturbances and disorders transcend demographic boundaries and can affect any patient, regardless of age, profession, socioeconomic status, education, race, or ethnicity,1,5,7 making the issue of sleep deprivation important for patient care across multiple medical specialties.
With a current membership of just under 6000 within the American Academy of Sleep Medicine and 1200 for Sleep Research Society,5 American Academy of Sleep Medicine,11 National Sleep Foundation,1 and Association of American Medical Colleges12 have predicted future physician shortages overall and in the field of neurology. In light of the epidemiological data on sleep disorder prevalence and the projected shortage of sleep specialists, the demand for sleep medicine will continue to exceed the supply of specialists. Consequently, other non-sleep specialists will be forced to fill this gap in patient care. However, most clinicians currently have between 15–22 minutes to discuss and manage their patients various medical conditions, ranging from heart disease, diabetes, obesity, and mental health.13,14 Thus, inclusion of sleep disorder evaluation and management into the clinical workflow of the non-sleep specialist calls for the application of additional time and cost-efficient clinical tools.
The introduction of mobile health (mhealth)15 serves as an untapped clinical resource tool for the non-sleep specialist caring for patients commonly at-risk for sleep conditions. Despite the potential benefit of mhealth tools in a clinical setting, few studies have investigated the use of the mobile platform to assist clinicians in clinical screening and diagnosis, facilitating communication and partnership with the patient, and improving patient outcomes.16,17,18,19 Thus, the need for a clinical (and educational) paradigm to address the sleep epidemic in healthcare is not only critical, but also time sensitive. To better equip clinicians managing patients with unmet sleep care needs, we developed an iPad® app to be implemented in the clinical workflow of non-sleep specialist clinics. The main aim of our study was to evaluate the feasibility of implementing the MySleepScript mhealth clinical tool across various established clinical workflows. As such, we specifically assessed the amount of time patients needed to complete app, patients’ satisfaction with using the app, and whether satisfaction using the app varied by patients’ characteristics (e.g., age, race, education).
Method
Study Protocol
Our study with the MySleepScript iPad® app was conducted from July 2014 to September 2015 across 5 non-sleep specialty Johns Hopkins outpatient clinics: neuro-Human Immunodeficiency Virus (HIV) clinic, movement disorders clinic, headache clinic, men’s health clinic, and multiple sclerosis clinic. Certified trained student research assistants conducted the study in these clinics. Each patient was approached by a study team member and consented using a standardized Oral Consent Script approved by the Johns Hopkins Institutional Review Board.
Healthcare Provider Preparation
Prior to utilizing the MySleepScript app in clinic, the clinician completed an interactive sleep educational iPad® app, MySleep101, created by our team. This app is made up of 10–15 minute interactive videos discussing the common presentations and treatment considerations for the following sleep disorders: Basic Sleep Concepts, Restless Legs Syndrome (RLS), Hypersomnia, Insomnia, Sleep Apnea, Circadian Rhythm Sleep Wake Disorders, Parasomnias, Post-traumatic Stress Disorder (PTSD) related sleep disturbances. MySleep101 was based on the Khan Academy® approach to deliver brief, high yield and engaging lectures focused on the identification and management of common sleep disorders. Users of this app learn about risk factors and symptoms associated with sleep disorder(s) of concern as well as behavioral strategies for managing them, under the guidance of the healthcare team. After viewing of the educational material and achieving a minimum score on the MySleep101 post-test, the MySleepScript app is “unlocked” for use by the provider.
Development of MySleepScript iPad® App
MySleepScript is an electronic clinical sleep app designed to assist non-sleep specialist clinicians in the evaluation and management in the outpatient setting. The MySleepScript clinical app encompasses a variety of standardized surveys mixed with other pertinent questions relating to sleep in an algorithm with built in logic depending on the entered responses. The validated surveys within the app include: The Pittsburgh Sleep Quality Index,20 Insomnia Severity Index,21 The Patient Health Questionnaire,22 Berlin,23 PTSD,24 RLS,25 and Perceived Neighborhood Disorder Scale Survey.26 Furthermore, questions developed by the sleep experts were included to target RLS, circadian rhythm disorders, parasomnias, and PTSD-related sleep disturbances. Questions from the JH Sleep Environment Inventory, created by the group to identify potential environmental contributors to poor sleep, were used as well. These surveys and questions were grouped and categorized into five sections accordingly: “Sleep Habits and Behaviors,” “Sleep Environment,” “Sleep and Neighborhood,” “Stress Level,” and “Sleep Attitudes.” Demographic information and “Sleep Habits and Behaviors” are mandatory for every patient to complete while the other sections are optional and completed depending on the provider’s prior selection of preferred questionnaires. For our study, patients completed the following three questionnaires – Demographics, “Sleep Habits and Behaviors,” and “Sleep Environment.”
Based on the patient’s responses, MySleepScript provides the clinician a “level of concern,” initiates an automated referral to the sleep specialist (if appropriate), and generates a customized educational PDF document (Figure 1) for the clinician/healthcare team to discuss and/or give to the patient to take home. Of note, MySleepScript does not diagnose patients with a sleep disorder, but rather identifies potential sleep concerns for particular sleep disorders so that clinicians already trained with MySleep101 educational app can explain the concern for a potential sleep disorder, refer or order tests (if decided by the clinician), and/or provide patient education. Clinicians have the opportunity to educate the patient regarding individual risk factors, discuss behavioral modifications, and provide a document stating these points as well.
Figure 1: Customized sample educational sleep document.
Study Workflow
We allowed each clinician team leader to determine the integration of the app into the clinical workflow allowing for flexibility. In the movement disorders clinic and men’s health clinic, patients were asked to participate in the study before having been seen by their provider. In the HIV, headache, and multiple sclerosis clinics, patients were approached immediately after their clinic visit. In either case, the results of the MySleepScript app were reviewed with the clinician and patient upon completion of the app. Patients also had the opportunity to read and receive via email the customized educational script. After this experience, each patient was then asked to fill out the satisfaction survey on paper. The two models of the study protocol are illustrated in Figure 2.
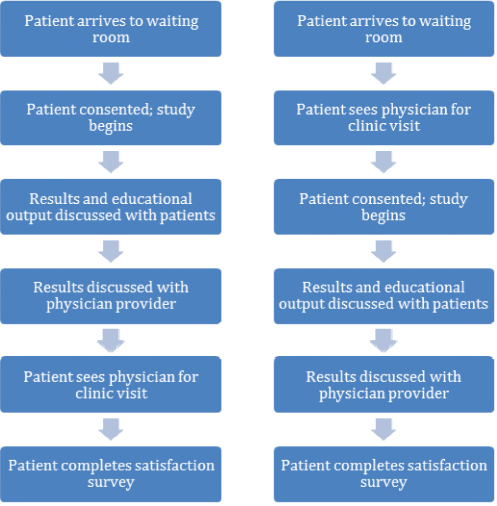
Figure 2: Study protocol
Patient Satisfaction Survey
In order to assess feasibility of using this tool in the clinical setting, our team developed a short satisfaction survey that each patient completed after using the app. This satisfaction survey was administered on paper and was completely distinct from the questions in the app assessing sleep. The survey featured seven questions–six that used a five-level Likert scale (strongly disagree to strongly agree), and one that used a yes/no format question. The Likert survey asked the following questions: “I found the MySleepScript app easy to use,” “I prefer completing questionnaires like this rather than paper versions,” and “I am happy my healthcare provider is using this app.” The question “Compared to previous visits with this provider, I feel that MySleepScript enhanced the quality of this visit” was only completed by follow-up patients. The yes/no question asked, “Would you recommend that your provider continues to use this MySleepScript app”. The results of the satisfaction surveys were entered into a database. Answers to Likert scale questions were assigned a value one through five, with “strongly agree” as “1” and “strongly disagree” as “5,” while “yes” as “1’ and “no” as “0.”
Data Analysis
The results from the satisfaction surveys, time to completion, and demographics were the primary outcome data analyzed in this study. Descriptive statistics were conducted to quantify whether or not a majority reported favorable responses to the MySleepScript satisfaction survey items. Independent samples t-test was conducted to examine whether responses on the continuous satisfaction survey items differ between new and follow-up patients. For the dichotomous satisfaction survey item, a chi-square test was conducted. T-tests and chi-square tests were conducted to determine if there were demographic differences with respect to satisfaction survey answers.
Results
From July 2014 to September 2015, 120 patients were enrolled in the study across 5 clinics (see Table 1). The study included 64% follow-up patients and 36% new patients. The majority of our patients were male (80%). Most of the patients identified as White (62%), followed by Black (28%), Asian (3%), and Latino (2%). The average age was 57±14. The majority of patients (87%) completed the app in less than 20 minutes, but a substantial percentage (66%) of patients completed the app in less than 15 minutes (Table 1).
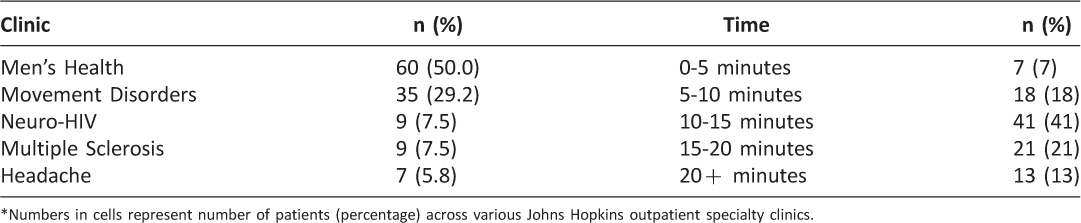
Table 1: Number of patients (n = 120) in clinics & time to completion
High Percentage of Patients Reported Satisfaction with MySleepScript
Ninety-one percent of the patients recommended that their health provider continue to use the MySleepScript app in their clinic. A majority of patients strongly agreed/agreed that the app was easy to use (94%), preferred the app compared to paper formats (78%), felt the app improved communication with their practitioner (83%), and provided helpful output for them as patients (65%). Overall, 85% of patients reported that they were glad their health provider was using the app (see Table 2).
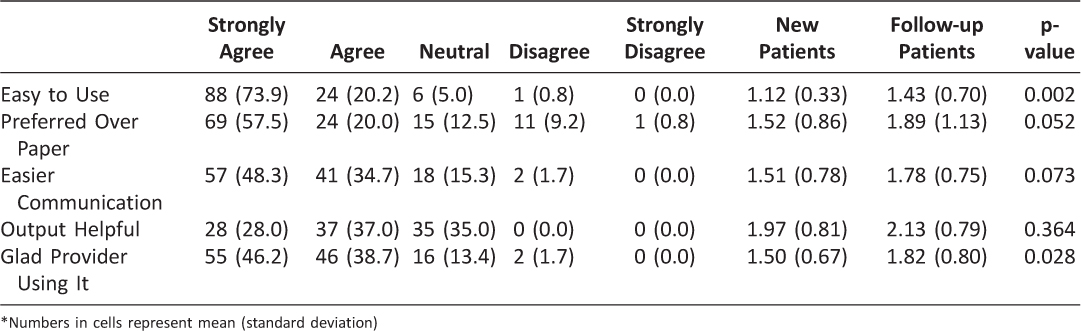
Table 2: Number (frequency) of patients’ responses to each satisfaction survey item
MySleepScript Satisfaction Report Differences across Patient Characteristics
No significant differences across patient characteristics (i.e., age, sex, race, education, and employment status) were observed for the satisfaction survey responses regarding ease of use, preference over paper, or recommendation to continue using app. No significant demographic differences were found between new and follow up patients. No significant differences across the patient characteristics (i.e., age, sex, race, education, and employment status) were observed for the time taken to complete MySleepScript.
More non-White patients (80%) than White patients (41%) (p = 0.009) reported that they strongly agreed that the MySleepScript was an easier form of communication. More non-White patients (60%) than White patients (16%) (p = 0.001) also reported that they strongly agreed the MySleepScript provided valuable output, and more non-White patients (76%) than White patients (35%) (p=0.004) strongly agreed they were glad the provider was using the MySleepScript app
Furthermore, more full-time working patients (74%) than unemployed (0%), retired (32%), or disabled patients (33%) (p=0.008) reported that they strongly agreed the app was an easier form of communication. More patients 40-64 years of age (52%) compared to patients 20-39 years of age (29%) and ≥65 years of age (15%) (p=0.018) reported that they strongly agreed the MySleepScript provided valuable output.
A significantly higher percentage of new patients (100%) than follow-up (88%) patients recommended that health practitioners should continue to use the MySleepScript app (X2 (1) = 5.15, p = 0.02). As illustrated in (Table 2), new patients were also significantly more likely than follow-up patients to report the app was easy to use (new patients mean = 1.12 (SD = 0.33) (follow-up patients mean = 1.43 (SD = 0.70); t (111) = 3.21, p = 0.002) and were glad the practitioner was using the app (new patients mean = 1.50 (SD = 0.67) (follow-up patients mean = 1.82 (SD = 0.80); t (114) = 2.22, p = 0.028). Among the follow-up patients, a high percentage reported they strongly agreed/agreed (66%) that the app enhanced the quality of their practitioner visit.
Discussion
Our team developed the MySleepScript iPad® app to equip clinicians with a patient friendly, time-efficient clinical tool to help in the evaluation of patients experiencing sleep disturbances. With mhealth platforms improving communication and healthcare across a variety of specialties and benefitting clinicians,16,27,28 their use have already become quite ubiquitous. For example, 85% of faculty physicians and 90% of residents use their mobile phones in clinical settings.29 However, this mhealth utilization is generally limited to tools such as medical references, drug information, and calculators.29MySleepScript represents an innovative utilization of the mhealth platform, especially from the standpoint of sleep healthcare, in its ability to equip the clinician with a resource to assist with the evaluation, management, and education of sleep disturbances/disorders.
Our goal was to assess patient satisfaction, patient characteristics, and time to completion across various established clinical workflows to evaluate the feasibility of implementing MySleepScript. With the increase in technology in recent years, many clinicians are cautious of introducing mhealth into their practice due to the fear of patient resistance, patients’ lack of experience with technology, and disruption of provider-patient communication.17,18,30 Supporting this, one study revealed that 20% of physicians reported “patients’ resistance to technologies” as a reason for their own skepticism.31 Thus, in order to for clinical mhealth technologies to be successful, it is imperative to demonstrate that patients are willing to use and can benefit from these technologies. Our data show that the majority of patients across a variety of demographics and clinical cohorts embraced the incorporation of mhealth tools into the clinical workflow, finding it easy to use and superior to the traditional format of filling out paper questionnaires. Furthermore, our results suggest that the degree of enthusiasm for mhealth tools was significantly higher among specific demographics, particularly middle aged, employed, and non-White patients. Such unique spikes in enthusiasm may warrant further exploration since mhealth may serve as a targeted strategy to enhance patient outreach and close potential health disparity gaps that may exist.
Interestingly, 83% of patients in our study believed that using the app enhanced communication between the provider and patient. Many skeptics caution that new health technologies could erode the doctor-patient relationship and diminish personalized care.30,32,33 Some evidence suggests that the use of Electronic Health Records (EHRs) has impacted critical components of patient-provider interaction and communication.33 Since patients in our study completed the app prior to their face-to-face encounter with the clinician, the use of this app likely did not negatively impact communication in the same manner as EHR documentation during a clinic visit may. Though our survey did not describe how exactly the MySleepScript experience helped to enhance the communication between clinician and patient, our data show that patients using MySleepScript reported the improvement in communication.
Based on individual questionnaire responses, MySleepScript produces customized educational output in the form of a PDF handout to each patient depending upon their responses to the questionnaires. Our results show that 65% of patients found this customized material helpful. Empowering and partnering with the patient is a core principle of clinical care,34 and personalizing educational materials for each patient provides an opportunity for patients to be involved in their care. This approach contrasts with the “one-size-fits-all” educational method often used in brochures, online healthcare education websites, and pre-printed paper information sheets.
One advantage of an iPad® app is that it can be completed at a variety of different time points and locations during the clinic visit, and including prior to being roomed for their visit while sitting in the waiting room. The waiting room has already been accepted as a medium for health education and patient engagement.35,36 Gilliam et al have successfully implemented an iPad® app in waiting rooms on contraception education with initial positive results on satisfaction and effectiveness.36 Our results also showed that 66% of patients completed the app within 15 minutes and 87% completed within 20 minutes. No significant differences were observed across participant characteristics (i.e., age, sex, race, education, and employment status), suggesting that this app may be completed by a variety of patients in a timely manner. Considering the average waiting room time in 2014 was 23 minutes,37 implementing this app in waiting rooms may serve as a resourceful use of the patients’ time.
One of the main reasons physicians adopt new technologies is to use time more efficiently.31 This app’s ability to automatically calculate scores for a number of surveys instantaneously allows for real-time inclusion of the results into the patient visit and treatment plan. Furthermore, this app can improve record keeping for completed surveys and in the future could allow for further integration with patient medical records and health portfolios. For the two clinics where the app was administered preceding the patient’s scheduled clinic visit (i.e., Urology/Men’s Health; Movement Disorders), providers did not report any issues or concerns with respect to clinic flow. However, provider attitudes were not directly measured in this study and serves as a future direction for further analysis.
Our study is not without limitations. Though we had encouraging satisfaction scores, our results included 120 patients in only 5 subspecialty clinics. Furthermore, the majority of our patients were male (80%) with an average age of 57 years. With the large diversity in outpatient clinic types, locations, specialties, populations served, and workflow, our conclusions are not necessarily applicable to every outpatient clinic. Moreover, our study is subject to selection bias, as the 5 clinics were not randomized and were pre-selected based on opportunities to conduct the study. Thus, the observed patient satisfaction ratings with the MySleepScript may not be generalizable across adult communities and academic clinic settings. Though providers reported no issues with respect to clinical workflow, follow-up studies should be completed to truly assess the perspectives of clinicians and their clinical administrative healthcare team using this app. Obtaining provider satisfaction and perspectives is critical in assessing what value, if any, does the app add to the clinician. While patients provided high satisfaction scores in using this app, it is unclear what, if any, measurable direct benefit this app brings to patient care. Although this app has a built-in customized educational component and assists clinicians in the assessment and management of patients with sleep issues, the impact on patient outcomes and clinical follow-up rates as a result of this tool warrants further investigation.
Conclusion
MySleepScript is an electronic clinical tool designed to assist clinicians in the evaluation, management, and education of sleep disturbances. Further studies are warranted to determine the perspectives of providers and to investigate both the benefits and health outcomes of mhealth educational and sleep medicine clinical tools placed in the hands of a non-sleep trained specialist. Results of this study, however, demonstrate promise that this approach was well received by a diverse population of patients which serves as a fundamental step towards widespread application.
Conflict of interest
Authors report no conflict of interest.
Financial disclosure
Dr. Rachel Salas has entered into an agreement with UpToDate, Inc. and has been paid royalties for her contribution of medical articles for this publication. She has received less than $400.
She has received royalties from sales of the MySleep101 iPad app. She has received less than $75.
Dr. Charlene Gamaldo has entered into an agreement with UpToDate, Inc. and has been paid royalties for her contribution of medical articles for this publication. She has received less than $400. She has received royalties from sales of the MySleep101 iPad app. She has received less than $75.
Peter Dziedzic has received royalties less than $500 from Johns Hopkins Technology Ventures, a company that distributes products that are part of the one discussed in this paper.
Dr. Alyssa Gamaldo discloses that she is a co-investigator on a NIH grant, funded from 2015–2017. Chronic Stress as a Pathway to Health Disparities Grant #: NIHR03 AG050798-01.
Dr. Luis Buenaver has received royalties from sales of the MySleep 101 iPad app. He has received less than $5.
No disclosures for Ankur Doshi, Anthony Kwan, Seulah Choi, Annette Wang, Aadi Kalloo.
Acknowledgements
We would like to thank Johns Hopkins Center for Behavior Health for their grant to help fund creation of the application.
References
1. National Center on Sleep Disorders Research. National Institutes of Health Sleep Disorders Research Plan. NIH Publication No. 11-7820. 2011 Nov.
2. National Institute of Neurological Disorders and Stroke. Brain Basics: Understanding Sleep. National Institutes of Health. NIH Publication No. 08-3440-c.
3. Leger D. The cost of sleep-related accidents: a report for the National Commission on Sleep Disorders Research. Sleep. 1994 Feb;17(1):84–93.
4. Ellen RL, Marshall SC, Palayew M, Molnar FJ, Wilson KG, Man-Son-Hing M. Systematic Review of Motor Vehicle Crash Risk in Persons with Sleep Apnea. J Clin Sleep Med. 2006 April 15;2(2):193–200.
5. Institute of Medicine (US) Committee on Sleep Medicine and Research; Colten HR, Altevogt BM, editors. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington (DC): National Academies Press (US); 2006. Available from: http://www.ncbi.nlm.nih.gov/books/NBK19960/
6. Connor J, Norton R, Ameratunga S, et al. 2002. Driver sleepiness and risk of serious injury to car occupants: Population-based case control study. BMJ. 2002 May 11;324:1125.
7. Hasler G, Buysse DJ, Klaghofer R, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004 Jun 15;27(4):661–6.
8. National Commission on Sleep Disorders Reseaerch. Wake up America: a national sleep alert: a report of the National Commission on Sleep Disorders Research, submitted to the United States Congress and to the Secretary, US Department of Health and Human Services. Washington, DC. The Commission. 1993 Jan.
9. Hossain JL, Shapiro CM. The Prevalence, Cost Implications, and Management of Sleep Disorders: An Overview. Sleep Breath. 2002 Jun;6(2):85–102.
10. Ting L, Malhotra A. Disorders of Sleep: An Overview. Prim Care. 2005;32(2):305–18. ![]()
11. Dall TM, Storm M, Chakrabarti R, et al. Supply and demand analysis of the current and future US neurology workforce. Neurology. 2013 Jul 30;81(5):470–8.
12. IHS Inc. The Complexities of Physician Supply and Demand: Projections from 2013 to 2025, Final Report Prepared for Association of American Medical Colleges. 2015 Mar.
13. Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007 Oct;42(5):1871–94.
14. National Center for Health Statistics. National Ambulatory Medical Care Survey: 2012 State and National Summary Tables. Centers for Disease Control and Prevention. 2012.
15. Brinkel J, Kramer A, Krumkamp R, May J, Fobil J. Mobile Phone-Based mHealth Approaches for Public Health Surveillance in Sub-Saharan Africa: A Systematic Review. Int J Environ Res Public Health. 2014 Nov;11(11):11559–82.
16. Ventola CL. Mobile Devices and Apps for Health Care Professionals: Uses and Benefits. Pharmacy and Therapeutics. 2014 May;39(5):356–64.
17. Misra S, Lewis TL, Aungst TD. Medical application use and the need for further research and assessment for clinical practice: creation and integration of standards for best practice to alleviate poor application design. JAMA Dermatol 2013 Jun;149(6):661–2.
18. Ventres W. Electronic health records: Can we maximize their benefits and minimize their risks? Acad Med. 2012 Nov;87(11):1456–7.
19. Tam C, Sharma A. Mobile medical apps: to regulate or not to regulate? American Pharmacists Association. 01 Dec 2013. Available at: http://www.pharmacist.com/mobile-medical-apps-regulate-or-not-regulate.
20. Buysse DJ, Reynolds Cf, Monk TH, Berman Sr, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989 May;28(2):193–213.
21. Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001 Jul;2(4):297–307.
22. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a Brief Depression Severity Measure. J Gen Intern Med. 2001 Sep;16(9):606–13.
23. Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999 Oct 5;1313(7):485–91.
24. Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Thraikill A, Gusman FD, Sheikh JI. The Primary Care PTSD Screen (PC-PTSD): Development and operating characteristics. Prim Care Psychiatry. 2003;9(1):9–14. ![]()
25. Abetz L, Vallow SM, Kirsch J, Allen RP, Washburn T, Earley CJ. Validation of the Restless Legs Syndrome Quality of Life quesitionnaire. Value Health. 2005 Mar–Apr;8(2):157–67.
26. Ross CE, Mirowsky J. Disorder and Decay: The Concept and Measurement of Perceived Neighborhood Disorder. Urban Affairs Review. 1999 Jan;34(3):412–32.
27. Nasi G. Cucciniello M, Guerrazzi C. The Role of Mobile Technologies in Health Care Processes: The Case of Cancer Supportive Care. J Med Internet Res. 2015 Feb 12;17(2):e26.
28. Aungst TD. Medical applications for pharmacists using mobile devices. Ann Pharmacother. 2013 Jul-Aug;47(7–8):1088–95.
29. Google/Manhattan Research. Screen to Script: The Doctor’s Digital Path to Treatment. Google Physician Channel Adoption Study. 2012 June.
30. Frankel R, Altschuler A, George S, et al. Effects of exam room computing on clinician–patient communication: A longitudinal qualitative study. J Gen Intern Med 2005 Aug;20(8):677–82.
31. MedData Group. MedData Point Report: Physician Perceptions of Mobile & Connected Health Q2 2014. MedData Group, LLC. 2014.
32. Ventres W. Electronic Health Records: Upsides, Downsides, and Inside-Outsides on their way toward their use in clinical practice. Teach Learn Med. 2013;25(4):366–8. ![]()
33. Montague E, Asan O. Dynamic modeling of patient and physician eye gaze to understand the effects of electronic health records on doctor-patient communication and attention. Int J Med Inform. 2014 March;83(3):225–34.
34. Hook M. Partnering with patients-a concept ready for action. J Adv Nurs. 2006 Oct;56(2):133–43.
35. Gignon M, Idris H, Manaouil C, Ganry O. The waiting room: vector for health education? the general practitioner’s point of view. BMC Research Notes. 2012 Sep 18;5:511.
36. Gilliam ML, Martins SL, Bartlett E, Mistretta SQ, Holl JL. Development and testing of an iOS waiting room “app” for contraceptive counseling in a Title X family planning clinic. Am J Obstet Gynecol 2014;211:481.e1–8.
37. Bleustein C1, Rothschild DB, Valen A, Valatis E, Schweitzer L, Jones R. Wait Times, Patient Satisfaction Scores, and the Perception of Care. Am J Manag Care. 2014;20(5):393–400.

