mHealth Clinic Appointment PC Tablet: Implementation, Challenges and Solutions
Carol E. Smith, PhD, RN1, Ryan Spaulding, PhD2, Ubolrat Piamjariyakul, PhD, RN3, Marilyn Werkowitch, BSN RN4, Donna Macan Yadrich, BS, MPA5, Dedrick Hooper, BS6, Tyson Moore, BSN, RN7, Richard Gilroy, MD8
1School of Nursing and Preventive Medicine & Public Health Department, University of Kansas Medical Center; 2Center for Telemedicine and Telehealth, Interim Associate Vice Chancellor, Institute for Community Engagement, University of Kansas Medical Center; 3School of Nursing, University of Kansas Medical Center; 4School of Nursing, University of Kansas Medical Center; 5Interventionist, School of Nursing, University of Kansas Medical Center; 6Center for Telemedicine and Telehealth, University of Kansas Medical Center; 7School of Nursing, Children’s Mercy Hospital, University of Kansas Medical Center; 8Department of Gastroenterology and Hepatology, University of Kansas Medical Center
Corresponding Author: upiamjariyakul@kumc.edu
Journal MTM 4:2:21–32, 2015
Background: Patients requiring daily intravenous (IV) home parenteral nutrition (HPN) would benefit from in-home professional observation to improve self-care, to assess, detect and prevent serious complications.
Aims: The study aims are to assess the viability and utility of conducting mobile healthcare (mHealth) videoconference assessments with patients managing lifelong daily 12-hour IV nutrition infusions in their homes. The challenges and solutions to implementing mobile personal computer (PC) tablet based clinic appointments are described.
Methods: A wireless Apple iPad Mini™ mobile touch-screen tablet computer with 5 mega-pixel camera was loaned to patients. Each tablet had Polycom RealPresence software and a fourth generation (4G) mobile telecommunications data plan. These supported audio-visual mobile videoconferencing encrypted connections between health professionals in their offices and HPN patients and their family members in their homes. Patients’ and professionals’ evaluations of their mHealth clinic experiences are collected.
Results: Patients (mean age = 41.9, SD = 2.8 years) had been prescribed 12-hour home parenteral nutrition (HPN) infusions daily due short bowel disorders. Patients had been on HPN from 1 to 10 years (M = 4, SD = 3.6). Evaluation of clinic appointments revealed that 100% of the patients (n = 45) and the professionals (n = 6) indicated that they can clearly hear and easily see one another. The mHealth audio-visual interactions were highly rated by patients and family members. Professionals highly rated their ability to obtain a medical history and visual inspection of patients. Several challenges were identified and recommendations for resolutions are described.
Discussion: All patients and professionals highly rated the iPad mHealth clinic appointments for convenience and ease of communicating between homes and offices. An important challenge for all mHealth visits is the clinical professional’s ability to make clinically accurate judgments about what they observed and heard from the patients. Following our solutions for obtaining clear visuals with the iPad can improve ability to make clinical assessments.
Introduction
There are two million patients requiring numerous types of home intravenous (IV) infusions,1–3 which leads to millions of dollars spent annually on complex IV home-care therapies that are administered by patients and their families.4,5 Notably, one of our nation’s most costly but preventable complications in IV therapy are bloodstream infections, a top 25 NIH research priority.6 Many thousands of people also require lifelong IV home parenteral nutrition (HPN) to survive the consequences of short bowel syndrome. As survival on long-term HPN has increased in this population,7,8 there is an estimated national cost of $2.3 billion per year.9–11 Even though HPN is life-saving, impaired quality of life and significant morbidity and even mortality accompany such long-term use.12,13 IV catheter-related bloodstream infection (sepsis) is the 6th leading cause of U.S. death in patients and is a significant cause of mortality associated with HPN.14
HPN patients often reside some distance from the few centers with health specialists specifically designated to manage long-term HPN care. Patients often travel many hundreds of miles for their specialists and are known to need care advice frequently.15 Thus there is an urgent need for testing mobile-based long distance health care options.16
Aims
This study tests mobile health (mHealth) defined as “the delivery of healthcare services via mobile communication devices.”17,18 The aims of this study are to assess the viability and utility of videoconference assessments of HPN patients. The results of the mHealth assessments are described,19 and the patients’ and professionals’ evaluations of the mHealth clinics are reported. We also describe the challenges and solutions found in implementing mHealth clinics using PC tablets with HPN patients at home by a health care team.20
Methods
The University of Kansas Medical Center (KUMC) Institutional Review Board (IRB) reviewed and approved this study protocol (#13337) before recruitment. All patients and family members signed an informed consent to participate. Recruitment of subjects was from our University Medical Center, associated rural health centers, and from the Oley Foundation, a 501(c)(3) support organization for HPN patients and their families. To control for heterogeneity of the sample, only patients on HPN for short bowel disorders (and not for malignant disease) and their family members were enrolled. Inclusion criteria for all subjects were alert and oriented, and able to read and write English and provide informed consent. Exclusion criteria were conditions such as disability disorders that prevent iPad use. Subjects were enrolled regardless of socioeconomic status, race, ethnic background, or gender.
All professionals involved in the clinic or observational review have IRB Human Subjects training and have signed confidentiality statements. Patient evaluations of the mobile intravenous access care (IVcare) clinic data are only reported in aggregated form, and no individual data is disclosed. A Data Safety and Monitoring Committee of telemedicine experts, HPN physicians and a statistician external to this project have approved our methods and continue to review and approve the procedures and data collected. The mobile clinic and subjects’ anonymous questionnaire evaluation data were obtained through encrypted secure connections and all data are stored behind the institutional firewall. Our secure servers have encrypted log-on codes and a password which provides each participant identity and data security per the Health Insurance Portability and Accountability Act (HIPAA).
A wireless touch-screen mobile Apple iPad Mini™ tablet with a fourth generation (4G) unlimited data plan for internet access was selected for the testing of the mHealth clinic appointments. Teleconferencing and encryption software were used for two-way audiovisual connections between health professionals in their offices and IV patients and family members in their homes.
Wireless Mobile PC Tablet and Data Plan
The iPad Mini high-definition, 5 mega-pixel, forward-facing built-in camera allows patients to take and send a picture or video to health professionals for assessment (e.g., of an IV site, ostomy site, or other problematic wound or fistula site requiring professional evaluation). The data plan for each iPad Mini is provided at no cost and the iPad Mini is loaned to patients during the study. This data plan provides real-time interactive videoconferencing via Polycom RealPresence software among multiple health professionals from their offices with IV patients and their family members at home. The iPad Mini has the screen space to accommodate up to six participants simultaneously with each in a “window,” so all are visible to one another.
IVcare Clinic Appointments via Mobile mHealth
The Center for Telemedicine and Telehealth systems coordinator mails the iPad Mini (with illustrated instruction manual) overnight to the homes. He contacted each family to provide assistance for the infrequent iPad connectivity problems (i.e., “dropped calls”) during the mHealth clinic appointments.
The mHealth clinic consists of a scheduled iPad videoconferencing appointment for patients and their family members to interact with health professionals who are experienced in HPN care and/or chronic illness management. Each mobile clinic appointment began with greetings and introductions, privacy clarification, and review of Health Insurance Portability and Accountability Act (HIPAA) regulations. Following introductions, two health professionals (a master’s prepared patient educator experienced with HPN and a mental health clinical specialist) presented HPN care self-management guidelines and facilitated discussion of topics related to HPN homecare challenges.
Mobile Visual Assessment
During the next step of the mHealth clinic appointment, patients were asked questions related to their medical illness, and an individual patient visual inspection was conducted. These steps coincide with a physician’s typical clinic appointment using specific health history questions and a visual physical assessment. The specific health history questions designed by a physician with extensive experience with this patient population are listed in Table 1. As stated in the informed consent form, all patients are asked to volunteer to show a close-up view of their IV site and, if present, their abdominal scars, ostomies, fistulas, or wounds.
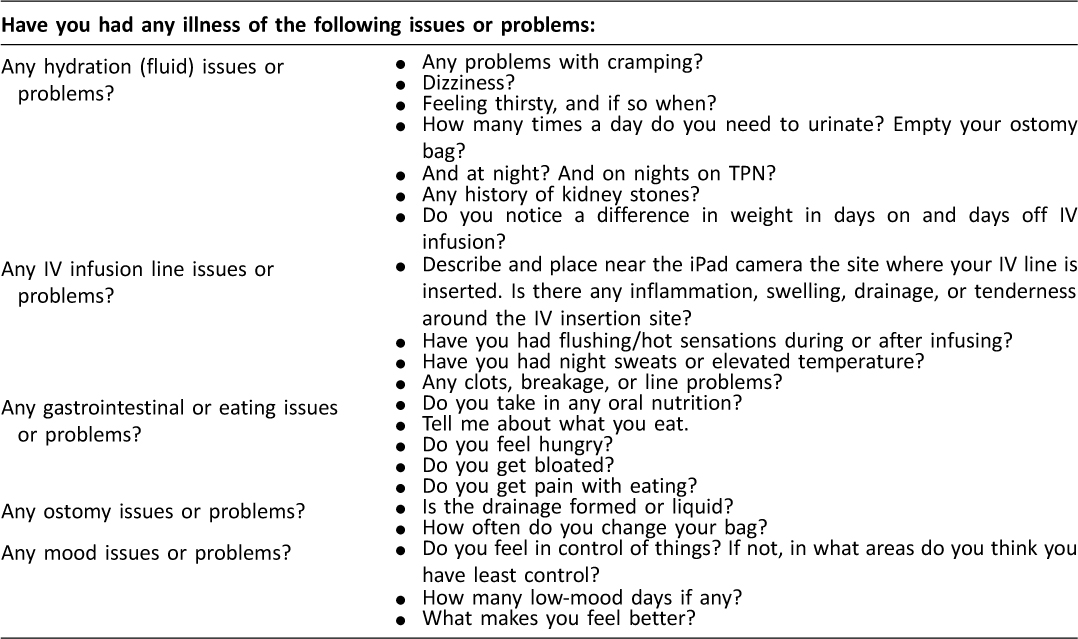
Table 1: Medical questions asked at routine mHealth clinic appointments.
These visual observations allow clinicians to assess each patient’s IV and abdomen site for skin integrity, color, and any drainage. Such visual assessments are standard components of an in-office physician appointment with these patients. Video recordings were made of patients’ IV insertion sites and abdomen sites. Then a second professional reviewed these videos and gave their independent ratings. This provided quality testing for agreement between professional clinical judgments based on two separate observations.21
Results
Sample
This HPN 45 patient sample (mean age = 41.9, SD = 2.8 years) consisted of chronically, but not fatally, ill patients who must travel significant distances (most with overnight stays) for specialists’ appointments. For survival most of these patients require daily 12-hour IV infusions due to a variety of lifelong short bowel disorders. The majority of subjects required lifelong HPN due to a diagnosis of bowel syndrome (64.9%) or motility disorders (30.4%). The duration on HPN in these patients was 1 to 5 years (61%), 6 to 10 years (26%), and more than 10 years for the remainder. Almost all (91.3%) routinely infuse HPN on 5 to 7 days per week.
The types of HPN catheter access for these patients included Hickman-Broviac (60. 8%), PICC line (26.1%), implanted device port (17.4%), or a surgically tunneled catheter (4.3%). IV access for over half of the patients had double lumen IV infusion catheters, and with those catheters 82.6% of the patients used one dedicated lumen for both medication infusion and blood draws. Ten participants had an ostomy, eleven had enteric tubes, and one had an abdominal fistula. Patients indicated that 68.1% had used a handheld computer devise, 70.3% used smartphones or similar touch screed devises and 97.8% had a home personal computer with internet connection.
Use of mobile PC tablets to conduct clinic appointments from a distance
Each of the 45 patients had two mHealth clinics appointments. According to our call list records, all but two patients attended at their initial scheduled clinic appointment time. The median interval between patients’ appointments was 2 months. These HPN patients learned to connect and to use the iPad Mini prior to the clinic appointments. The technician telephoned each patient to establish a connection prior to the appointment. Of the 45 patients, all indicated the illustrated training pages attached to the iPad and the on-line video demonstration were clear. However, 12 patients needed additional telephone guidance for connecting the day of the appointment.
For patients who could position the camera close to their IV insertions, fistulas, scars/incisions, ostomy sites, and gastrostomy tubes, the iPad Mini visual observations of the abdominal area allowed for assessing these sites. Each individual clinic video recording had a time stamp of the patient’s visual exam. This time stamp allowed the secondary professional reviewer to readily access that specific patient’s video recording. The secondary professional reviews rated the HPN patient’s iPad Mini video recording of these clinic appointments and agreed (88%) with the original health professional’s assessment and clinical judgment. This percent agreement is similar to agreements reported between multiple professionals’ in-person assessments.22
The frequency of patients’ concerns discussed during the appointments included: patients’ needs for informal peer and formal professional support (n = 12); trying to achieve an everyday sense of normal (n = 4); infection prevention (n = 3); low moods (n = 3); fatigue (n = 4); and avoiding hospitalizations (n = 2).
Patient, Family Member, and Health Professional’s Evaluation of the mHealth Clinics
Overall to date, the mHealth clinic appointments via iPad Mini were evaluated by all professionals, patients and family members (n = 72). These evaluations were collected from surveys emailed to the participant’s iPads and completed on-line at our encrypted firewall-protected data collection site. See Table 2 for the rating results for each evaluation survey question.
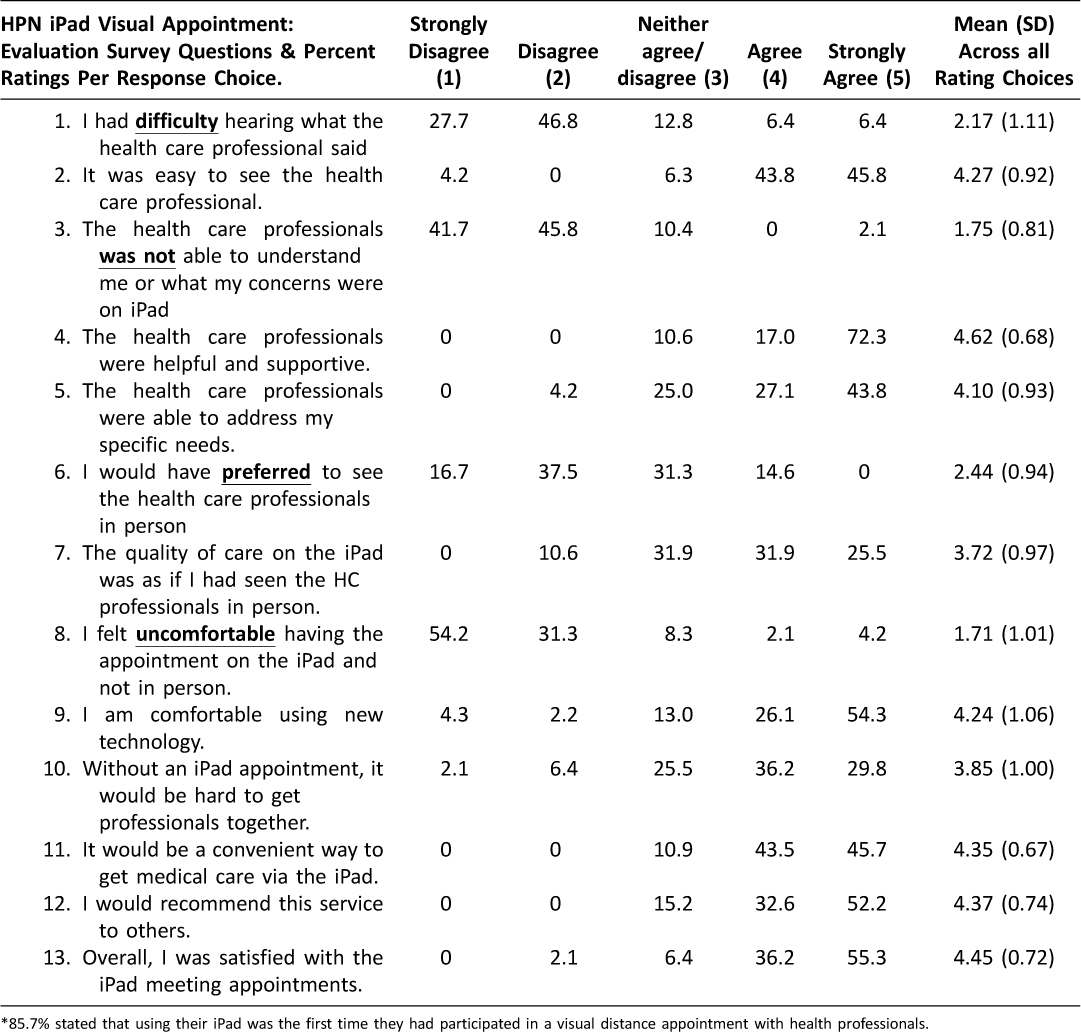
Table 2: HPN Patients and Family Members Visual Appointment Evaluation Survey Questions (each responder had 1 or more iPad clinic appointments)*
The majority of discussed responses to the survey: (1) mHealth clinic appointments were convenient; (2) we were able to hear clearly and “the professionals understand me and address my specific needs”; (3) the health professionals were helpful and supportive; (4) the quality of health care was as if I had seen the health professionals in-person; (5) the vast majority rated themselves as being comfortable having the appointment on the iPad versus in-person; and (6) indicated that without the iPad “getting my health care team together would be difficult”. Comments also indicated that the iPad could be used to teach HPN homecare, for post-surgery or hospital discharge follow-up, and that having the iPad tablet for contacting with their healthcare provider “is an advantage”.
Patients were asked to suggest which professionals they would want to attend PC tablet clinics. By rank order the patients selected their physician and HPN infusion team (i.e., nurse, dietician). In addition, mental health professionals, pain specialists, social workers, and payment specialists were also ranked as being helpful in mHealth clinic appointments. Likewise, professional evaluations were positive, rating the patient as easily observed and with “face-to-face” interactions as informative and easily conducted. Professionals noted visual blurs occurred occasionally but were easily fixed.
Patients Report Use of the iPad Mini for Many Aspects of Their Healthcare
Patients were asked about using the iPad Mini for other healthcare purposes. Patients reported sending photos of their IV site to their physicians. In the case of one patient who sent an iPad photo of his “itching and red” IV site, the physician suspected an early exit site stage infection and initiated an in-person visit. Other patients sent iPad photos of their required 24-hour urine collection containers. These photos allowed professionals to see the patients’ fluid output and to judge the urine color. Frequent fluid balance assessment is required in HPN patients and use of the iPad for clinic visits and transmitting photos of urine collection containers was reported by patients to save them repeated 60 to 150 miles of travel expenses and time for driving to the physician’s office. Other reasons why travel expenses were saved were reduced in-person appointments.
Other patients reported using their iPads during hospital stays to keep track of their own input and output, their changing of medical orders and laboratory values. The hospital nurses told the patients that “all HPN patients need the mHealth tablet to keep track of their complex daily care.”
Other patients reported using the iPad to: (1) track their medication, lab values, medical supplies, and fluid intake and output; (2) connect to the Oley Foundation patient advocacy website; (3) watch movies during the often long waits for in-person health procedures or examinations; and (4) use the iPad camera to more clearly visualize their own IV insertion site. One patient’s IV insertion site was under her clavicle and by observing the iPad screen she was able to zoom in and see it.
Challenges and Solutions in Implementing mHealth Clinics and Mobile IVcare
Using the iPad Mini for mHealth care clinic appointments posed technical and user challenges. Solutions to these challenges are described.
Connections
First, an expected challenge was when several patients (n = 8) contacted the systems coordinator for instructions on using their iPad Mini, while others reported having teenagers in their local area to help them. A common question among the 8 was how to find the on/off power button even though this was marked. Some patients (n=12) also required technical assistance each time they needed to make a connection for the session. The solution was to have our project technical team member assist them via telephone. Since the telemedicine systems coordinator was scheduled to be at each clinic appointment this was neither time consuming nor an added expense. The most common problem was among patients trying to make the connection using the dialing instructions included in the instruction manual. These instructions were simplified and found to solve this problem.
These technical assistance contacts were typically all short one-time telephone exchanges. Only one iPad had to be returned for reconfiguration, and that was due to a patient inserting a personal password code and then not being able to recall that password. This occurred only one time.
Technical Videoconferencing Software Challenges
The Medical Center maintains videoconferencing software that provides the iPads encryption; however this software could not be enabled outside of our Medical Center network. To address this issue, an additional firewall device was required to ensure encryption among the healthcare team and the patients at a distance. Another technical issue experienced late in the first year caused patients’ iPad mobile applications to shut down abruptly after 20 seconds in clinic appointment sessions. After follow-up with the internet data plan provider, it was determined that an update to their provider network was affecting the connections. The solution was to assign static Internet Protocol (IP) addresses to each device.
Another minor challenge was the occasional “dead spot,” or area of limited wireless service and the solution was simply asking the patient to move to another room or floor of the house to obtain a better signal. Several patients connected for the mHealth clinic appointments from locations other than their homes. Such connections from various locations and using the iPads for other health related contacts verifies the tablets were being used as mobile devises for health care.
Angles of View and Quality of Pictures
In regard to video and picture quality, dim lighting and glare from the transparent sterile bandage placed over the IV insertion site as protection, reduced the ability to visualize the IV site. Lighting sources from the side presented better images and did not cast a shadow. The types of light did not seem to impact the quality of the picture as much as the angle and distance from the lighting source. The solution was to instruct patients to move the iPad close to the source of light so that the glare was eliminated or diminished.
Another problem for visual inspection was the angle of the camera. For some patients this was the first time using the iPad, and they needed directions on how to place it to create the best angle for reducing glare and improving visualization. Often the camera was below or to the side of the IV site. Best visualization occurred when the patient had the camera level with the IV site. Camera distance from the site created similar complications. When patients held the iPad or had the iPad resting on a stable surface at a distance greater than 12 inches, the professional was unable to accurately assess the IV insertion site for inflammation or swelling.
Stability of the Camera
Camera movement during the visualization process caused the image to become distorted. Movement of the camera also changes the zoom and focus of the iPad camera. A related issue was the time spent visualizing each site. At least 20 seconds of a steady iPad camera view of the IV or abdominal site was needed for clarity. Patients were reminded to remain as still as possible. Also, some sites were not available for observation due to gauze or tape bandages, BioPatch film, or non-transparent colostomy dressings. Requesting patients to remove dressings would be a sub-optimal solution when the IV sites are obstructed by dressings. Rather re-scheduling an iPad visual assessment at a time of the patients’ routine dressing change when they are using aseptic technique is a better alternative.
Voice Activated Screen Adjustment
The iPad screen is auto activated so that the screen will automatically enlarge the face of the speaker.23 When there are multiple persons (i.e. patient, multidisciplinary professionals, and family members) in a session, the image of the person who begins to speak is automatically enlarged on the screen so that other members can see the primary speaker. This became problematic in conducting the visual assessment if a family member spoke and the screen automatically moved off the IV site and onto the person speaking. It was therefore important to forewarn those participating about these automatic screen size changes; the health professionals instructed patients and family members not to speak or comment when the patient being assessed was showing their IV and abdominal sites. However, our IT technician subsequently changed the iPad settings so there is no longer automatic screen switching.
Staying in the Picture
Finally, another challenge was that patients sometimes needed instructions from the health professionals to better place the iPad camera and themselves within the video picture so that their IV insertion, fistulas or ostomy sites could be better seen. See Table 3 for the guidelines for greater visual clarity that we developed from our experiences.
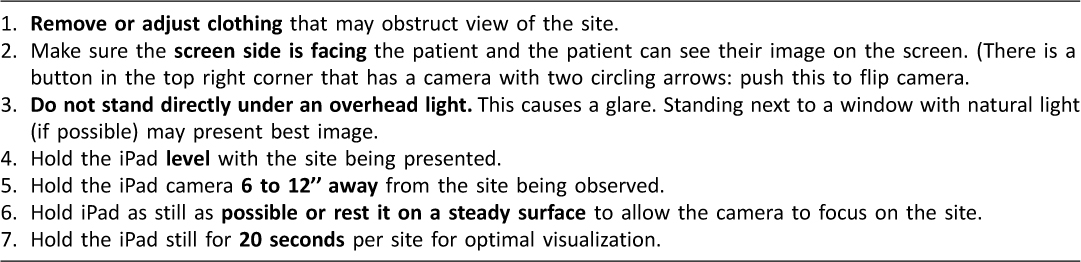
Table 3: Guidelines for Optimizing Observation of Patients per Mobile Tablet
Limitations
One limitation in this study was that not all iPads were returned to the clinic with all the peripherals. About 10 iPads were returned without charging cords. Another concern is the lack of person to person touch both in the handshake and the physical exam, which is not possible through this iPad approach. And without such touches initially establishing a therapeutic relationship with the patient may be a challenge. However, we have found with this population that obtaining expert experienced team information and guidance is always welcomed.
Another limitation to this study is the short timeframe for determining the scalable utility of the mHealth appointments, thus it is hard to determine how use of mHealth will be achieved in the future. In larger studies long-term telehealth clinics have become established as routine in our medical center (i.e. inner city school telehealth visits by pediatricians24 and oncology outreach).25 A current study with iPads and burn patients is now being conducted to determine the clinical judgment matches between iPad and in-person skin damage assessments. That study goals are to increase the ease and frequency of obtaining visual assessments, reduce travel and exposure to infection of burn patients served by our regional center. Our center’s has a 25 year long history of successful telehealth innovations including psychiatric home care counseling.26 Thus our physicians, nurses and mental health professionals understand the need to test new telehealth equipment, the importance of determining the viability of clinical assessments with specific populations and the advantages of the whole team meeting with the patient for a consistent clinical plan.
The professionals involved in this study had no negative concerns about the iPad visualization except when the IVs were obstructed by dressings and they could not assess the site. Also, the scheduling for the mobile appointments, as in other telemedicine clinics occurs, in the rooms established for such examinations. Not all team members participated at the scheduled time (although all came within 10 minutes). However, this was not seen as disruptive, as the professionals were pleased with the ease of using their own office. Negative evaluation comments from patients were limited to the few disconnections that occurred (all readily reconnected). And indeed 93.6% of these patients and their family members recommend the mHealth appointments to others.
Discussion
A majority of patients’ clinical problems were identifiable by a well taken history and a physical review, which is often observational in nature.27–32 HPN patients are a population in whom this paradigm holds true.33 Other studies have shown that telehealth communications have the same proportion if interpersonal and clinical dialogue as in-person appointments.34,35 Our clinical history assessment questions and discussions engaged the patients in sharing further understanding of their condition. Patients across most studies indicate preferences for in-person visits compared to telehealth or distance assessments. Although it was not only patients that were homebound or at a distance from care, that highly rated these iPad audio-visual contacts as positive.36
The utility of videoconferencing for HPN patients relates to ability of the professionals to conduct a health history and adequate visualization of the IV site and abdomen. The primary and secondary viewer rating of the clinical accuracy of the abdominal visual fields were comparable. The videotaping and storage of these iPad assessments also allowed for discussing the mHealth findings with colleagues. Our iPad appointments were rated by our health professionals as acceptable for patient’s clinical assessments with the caution that what can be clearly seen or not be seen should also be charted.
An important challenge for all mobile health-care is the clinical professional’s ability to make accurate health assessments and observations of patients. Future mHealth studies should be undertaken to test the viability of observing patients conducting their HPN care, such as using their IV ports.
Prevention of infection by professional supervision via iPad of catheter homecare technique is an important future study. What is also needed in the future for integrating mHealth are efficient coding systems in patients’ electronic medical records. Records should include charts for fluid balance, urine characteristic notes, and standard descriptions of vascular access sites, and surgical wound, or ostomies sites. This would allow for distance mobile clinic recorded observations and clinical data to be used as comparisons with future patient assessments. In addition, other mobile physical assessment tools can also be used such as electronic scales, vital signs, EKGs, and oximetry.
Observing for line sepsis on a frequent basis is critical. Videoconferencing can provide triage for signs or symptoms of infection and other catheter related problems and facilitate these solutions. These videoconference appointments allowed a clinical assessment of symptoms, exit site skin infection, and IV insertion site observation for inflammation. In instances where the physician must determine if there is a central line infection, an in-person visit for blood cultures is required. In this study, one patient presented with symptoms and visual signs of inflammation around the HPN infusion catheter site and was referred for an in-person visit. Infection detection often needs need follow-up in a hospital setting and management with an alternate IV access and antibiotics. Treatment instigation based on video-visual inspection alone is not recommended.
Cornerstones in clinical fluid balance assessment are: patient weight (which can be charted and tracked in mHealth); daily urine volume (which can be charted and quantities seen in mHealth; and ostomy output (which can weighted and tracked in mHealth). Weight changes can be monitored via mHealth through a linked weight scale and Bluetooth. In terms of fluid balance, the clinical assessment also can be initiated via videoconferencing. Also history data about dehydration was obtained in the teleconference including the presence or absence of edema or dry mucous membranes. In summary, the core clinical information used in a HPN clinic can be obtained with mHealth. When laboratory data is needed an in-person visit is required.
Telemedicine connections may not currently be right for every HPN patient.37 This being said, smartphones and tablets are now commonly being used by patients to contact professionals and to transmit data such as images. Unfortunately, these approaches do not have encrypted software to protect privacy, and professionals are being forewarned regarding these interactions.
Notably, mHealth carries important economic opportunities as hospitals face new economic consequences resulting from patient readmission and are incentivized on a fee-for-value basis.38 Also government and insurance incentives exist to increase remote monitoring systems with the goal of improving the quality of care in under-resourced areas while also minimizing the impact of the cost of travel for patients and their families.39,40 A 2012 study from the Brookings Institute found that remote monitoring technology could save nearly $200 billion for managing chronic diseases in the U.S. over the next 25 years.41 A significant advantage in this study is that our Medical Center has a low negotiated rate for all data plan coverage. 42 Such negotiations for data plans should be undertaken for all who are establishing mobile clinics for low cost, HIPAA alignment, and data encryption.
Mobile health innovations need to continue to be evaluated for meaningful-use and health data analytics.43 This project’s final outcomes could provide new information for: (1) biotechnology, by translating reliable “best practices” into mobile distance healthcare applications;44 (2) healthcare economics, by calculating the cost efficiency of a mobile system in ratio to in-person health services used; and (3) clinicians and administrators, by providing new distance care interventions for the large populations on home IV therapies who have three to five annual hospitalizations which might be prevented with mHealth follow-up.45
Conclusion
The mHealth clinic appointment can simultaneously connect multiple professionals and families on the iPad Mini screen. The data collected from patients’ provided important history and visual information for evaluating HPN patients’ clinical condition. And patients themselves transmitted photographs and videos for timely assessment of symptoms. This facilitated their care without increasing cost to the patient and saved them travel time. In our mHeatlh clinics technical issues were readily identified and solutions to resolve these were found.
mHealth advantages include early detection of infection, accurate assessment of IV insertion sites and/or detection of fluid balance issues through visual and history assessment of patients requiring HPN. The long-term goals of this study are to gain new knowledge about mobile management of complex chronic conditions using PC tablets.46 Mobile technology gives professionals an important opportunity for assessment of early symptoms and signs of IV infection or bowel illness exacerbations.
Funding Sources
The project is supported by the National Institute of Biomedical Imaging and Bioengineering (R01 EB015911), Carol Smith, Principal investigator. In addition, this study is partially supported by a Trail Blazer Award (awarded to Dr. Smith) from Frontiers: The Heartland Institute for Clinical and Translational Research, University of Kansas Medical Center (NIH U54 RR031295). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Biomedical Imaging and Bioengineering or the National Institutes of Health.
Acknowledgements
We are grateful for Chanawee Prinyarux, BComp; Brad O’Bryhim, MHSA, and Dennis Schukman for their technical expertise in establishing the iPad clinics. We acknowledge clinical expertise contributed to this study by Noreen Thompson, RN, MSN (adult mental health specialist); Eve-Lynn Nelson, PhD (pediatric mental health psychologist); and Heejung Kim, RN, PhD for her tabulation of mobile clinic costs. The authors extend their appreciation to all families who participated in this study for their time and evaluation of the mobile health care clinics.
References
1. Angus DC, Linde-Zwirbe WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome and associated costs of care. Crit Care Med 2011;29:1303–10. ![]()
2. Kelly DG, Tappenden KA, Winkler MF. Short bowl syndrome: highlights of patient management, quality of life, and survival. Journal of Parenteral and Enteral Nutrition 2014;8:427–37. ![]()
3. Howard L. Home parenteral nutrition: survival, cost, and quality of life. Gastroenterology 2006;130:S52–9. ![]()
4. Piamjariyakul U, Smith CE, Ross VM, Yadrich D, Williams AR, Howard L. Part I: HPN Complex Home Care: Utilization and Costs for HPN Health Care Services Each Year. Nursing Economic. 2010;28(4):255–64.
5. AARP Public Policy Institute (2009, November). Valuing the Invaluable: The Economic Value of Family Caregiving, 2008 Update. Washington, DC; 2009.
6. IOM. The Role of Telehealth in an Evolving Health Care Environment, 2012.
7. American Society for Parenteral and Enteral Nutrition. A.S.P.E.N. Launches a new online patient registry for nutrition support therapy. Available at: www.nutritioncare.org/News/ASPEN_New_Online_Patient_reigstry_Nutrition_Support_therapy/ Accessed June17, 2014.
8. Motodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel disease, based on systematic review. Gastroenterology 2012;142:46–54. ![]()
9. Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease incidence, prevalence, and environmental influences. Gastroenterology 2014;126:1504–17. ![]()
10. Wojtylak F. Medicare enteral and parenteral reimbursement: Requirements for successful coverage and payment. Support Line 2006;18(4):18–23.
11. Kelly DG. The clinician’s responsibility for the consumer’s financial well-being. Nutrition in Clinical Practice 2006;21(6):539–41. ![]()
12. Iyer KR. Surgical management of short bowel syndrome. Journal of Parenteral and Enteral Nutrition 2014;38:53–9. ![]()
13. Hofstetter S, Stern L, Willet J. Key issues in addressing the clinical and humanistic burden of short bowel syndrome in the US. Curr Med Res Opin 2013;29:495–504. ![]()
14. Dreesen M, Foulon V, Spriet I, et al. Epidemiology of catheter-related infections in adult patients receiving home parenteral nutrition: a systematic review. Clin Nutr 2013;32:16–26. ![]()
15. Piamjariyakul U, Yadrich S M, Ross VM, et al. Complex Home Care: Part II-Family Annual Income Insurance Premium and Out-of-Pocket Expenses. Nursing Economic 2010;28:323–9.
16. Saqui O, Chang A, McGonigle S, et al. Telehealth videoconferencing: improving home parenteral nutrition patient care to rural areas of Ontario, Canada. Journal of parenteral and enteral nutrition 2007;31(3):234–9. ![]()
17. Torgan C. The mHealth Summit: Local & Global Converge. Retrieved from http://www.caroltorgan.com/mhealth-summit/. Accessed on October 16, 2013.
18. Spaulding R, Smith, CE, Nelson EL, et al. iCare: mHealth Clinic Appointments Using iPad Minis Between Multiple Professionals and Intravenous Dependent Patients in their Homes; ATA Case Study. American Telemedicine Association. 2014. www.americantelemed.org/about-telemedicine/telemedicine-case-studies/case-study-full-page/kansas-icare-mhealth-clinic-appointments-using-ipad-minis-between-multiple-professionals-and-complex-patients-in-their-homes. Accessed 3/1/2014.
19. Seidner DL, Schwartz LK, Wiknler MF, Jeejeebboy K, Boullata JL, Tappenden KA. Increased intestinal absorption in the era of reduglitde and its impact on management strategies in patients with short bowel syndrome-associate intestinal failure. JPEN J Parenter Enteral Ntr 2013;37:201–11. ![]()
20. Tak SH, Benefield LE, Mahoney DF. Technology for long-term care. Res Gerontol Nurs Jan 2010;3(1):61–72. ![]()
21. Heinzelmann PJ, Willams CM, Lugn NE, Kvedar JC. Clinical outcomes associated with telemedicine/telehealth. Telemed J E Health 2005;11:329–47. ![]()
22. Nelson E, Miller EA, Larson KL. Reliability associated with the Roter Interaction Communications Analysis System adapted for the telemedicine context. Patient Education and Counseling. 2010;78(1):72–8. ![]()
23. Aslam TM, Murray IJ, Lai MYT, et al. An assessment of a modern touch-screen tablet computer with reference to core physical characteristics necessary for clinical vision testing. J. R. Soc Interface 2013;10:20130239. ![]()
24. Nelson E, Duncan A, Peacock G, Bui T. School-based telemedicine and adherence to national guidelines for ADHD evaluation. Psychological Services. 2012;9(3):293–7. ![]()
25. Doolittle GC. Spaulding AO. Providing access to oncology care for rural patients via telemedicine. J Oncol Prac 2006;2(5):228–30. ![]()
26. Doolittle GC, Spaulding AO, Williams AR. The Decreasing Cost of Telemedicine and Telehealth. Telemed J E Health 2011;17(9):671–5. ![]()
27. Smith CE. Testing Virtual Nurse Caring by Picture Phones and Internet with Home Parenteral Nutrition Patients. Clin Nutr 2007;2(2):43–4.
28. Grady B, Myers KM, Nelson EL, et al. Evidence-based practice for telemental health. Telemed J E Health 2011;17(2):131–48. ![]()
29. LinHanjun, HsuYeh-Liang, Ming-Shinn HsuMing-Shinn, ChengChih-Ming. Development of a Telehealthcare Decision Support System for Patients Discharged from the Hospital. Telemedicine and e-Health 2014; 20(8): 748–56. ![]()
30. Sistek D, Tschopp J-M, Schindler C, Brutsche M, Ackermann-Liebrich U, Perruchoud A-P, Leuenberger P, SAPALDIA team. Clinical diagnosis of current asthma: predictive value of respiratory symptoms in the SAPALDIA study. Eur Respir J. 2001 Feb;17(2):214–9.
31. Wang C, FitzGerald J, Schulzer M, Mak E, Ayas N. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA 2005;294:1944–56. ![]()
32. Call S, Vollenweider M, Hornung C, Simel D, McKinney W. Does this patient have influenza? JAMA 2005;293:987–97. ![]()
33. Bozzetti F, Forbes A. The ESPEN clinical practice guidelines on parenteral nutrition: present status and perspectives for future research. Clinical Nutrition 2009;28:359–64. ![]()
34. Nelson E, Bui TN, Velasquez SE. Telepsychology: research and Practice Overview. Child and Adolescent Psychiatric Clinics of North America. 2011;20(1):67–79.
35. Nelson E, Velasquez S. Implementing psychological services over televideo. Professional Psychology: Research And Practice. 2011;42(6):535–42. ![]()
36. Ronald C. Merrell and Charles R. Doarn. Disease Management in Telemedicine and e-Health. Telemedicine and e-Health 2014; 20(8): 679–80. ![]()
37. McCann E. mHealth to see big growth, barriers. Retrieved from: http://wwwhealthcareitnews.com/news/mhealth-see-big-growth-barriers. Accessed on 6/25/2014.
38. Mistry H, Garnvwa G, Oppong R. Critical Appraisal of Published Systematic Reviews Assessing the Cost-Effectiveness of Telemedicine Studies. Telemedicine and e-Health July 2014: 609–18 ![]()
39. Feinberg LF, Newman S, Gray L, Kolb K. The State of the States in Family Caregiver Support: A 50-State Study. San Francisco, CA: National Center on Caregiving at Family Caregiver Alliance; 2008.
40. Trapollo LLC Teams with Humana Cares for Landmark Telehealth Deployment to 1600 Humana Subscribers, PR Newswire. 2012. Retrieved from: http://www.prnewswire.com/news-releases/trapollo-llc-teams-with-humana-cares-for-landmark-telehealth-deployment-to-1600-humana-subscribers-145739995.html
41. West DM. How mobile devices are transforming healthcare. Retrieved from: http://wwwbrookings.edu/research/papers/2012/05/22-mobile-health-west. Accessed on 2/25/2014.
42. Kim H, Spaudling R, Werkowitch M, Yadrich D, Piamjariyakul U, Gilroy R, & Smith CE. Costs of multidisciplinary parenteral nutrition care provided at a distance via mobile tablets. Journal of Parenteral and Enteral Nutrition, 2014. doi: ![]() .
.
43. Smith CE, Piamjariyakul U, Yadrich DM, Ross VM, Gajewski B & Williams AR. Complex Home Care: Part III-Economic Impact on Family Caregiver Quality of Life and Patient’s Clinical Outcomes. Nursing Economic$ 2010;28(6):393–9, 414.
44. Smith C. Improving home care: virtual nurse caring. International Research Innovation Reports. May 2010:102–5.
45. Skiendziel P, Tanner, J, Hitchen, K, Korpolinski, R, Bodkins, T, Canfield, S, Bass, D. (2011, February). Multidisciplinary education and communication are critical for safely initiating parenteral nutrition in the home. NCP, 2011: 2:26(1) 22–4.
46. Baker TB, Gustafson DH, Shah D. How can research keep up with eHealth? Ten strategies for increasing the timeliness and usefulness of eHealth research. J Med Internet Res. 2014 Feb 19;16(2):e36. doi: ![]() .
.

