3D Printed Smartphone Indirect Lens Adapter for Rapid, High Quality Retinal Imaging
David Myung, MD, PhD1, Alexandre Jais, MS1, Lingmin He. MD, MS1, Mark S. Blumenkranz, MD1, Robert T. Chang, MD1
1Byers Eye Institute at Stanford, Stanford University School of Medicine, Stanford, California
Corresponding Author: viroptic@gmail.com
Journal MTM 3:1:9–15, 2014
Obtaining a secure, photographic record of clinical findings during patient encounters can serve as a powerful adjunct to the otherwise text-heavy documentation that dominates modern electronic health record systems. This is particularly true in ophthalmology, which is one of several medical specialties that relies heavily on images for diagnosis and treatment. Conventionally, ophthalmic imaging has required expensive, tabletop units operated by a trained technician in an outpatient clinic setting. The ubiquity and evolution of smartphones into both high-resolution cameras and conduits for encrypted data transfer has the potential to change this; however, their use is inherently limited by the optics and lighting required to image the eye, and in particular, the retina. Here, we report the development of a lightweight, compact, user-friendly, 3D printed attachment enabling high quality fundus photos by coupling smartphones to indirect ophthalmoscopy condensing lenses. The attachment is designed to hold a specific lens at a prescribed but adjustable distance from the camera lens, can utilize either the phone’s native flash for lighting or another coaxial light source, and has the potential to be operated with one hand. Using both mechanical prototypes and subsequent 3D printed versions of the device, we were able to photodocument a variety of both normal and abnormal retinal findings.
Introduction
Image-capture in ophthalmology is used extensively for disease documentation, treatment monitoring, and education. Traditionally, this has relied upon expensive, tabletop units operated by a trained technician in an outpatient clinic setting. The pervasive adoption of smartphones by physicians and the ever-improving built-in camera technology has spurred much interest in their use for ophthalmic imaging. These developments, along with improvements in cloud storage, electronic medical records accessible by smartphone, and encryption technology, now present the opportunity for a wholly smartphone-based teleophthalmology system.
In January 2013, the FDA approved the iExaminer (Welch Allyn, Skaneateles Falls, NY), the first smartphone-based imaging adaptor system that attaches an iPhone 4 (Apple Inc, Cupertino, CA) to Welch Allyn’s Panoptic Ophthalmoscope to capture images of the retina in combination with the iExaminer App. Before iExaminer, several groups had created various slit lamp adaptors that could also capture retinal images.4 More recently, investigators have published on results of using smartphones in conjunction with indirect ophthalmoscopy condensing lenses, a standard examination technique familiar to all eyecare providers.3, 5–7 Of note, Haddock et al.5 identified an iPhone application that allows control of the native flash as an adjustable light source, which reduces its light intensity to safe levels for indirect ophthalmoscopy.5, 8
Our group has also been exploring various technologies and approaches to smartphone-based fundus photography, with a particular focus on how to do so without adversely impacting clinical workflow. To this end, we have sought to develop a way for practitioners to more easily image the retina with their smartphones without the need for a slitlamp or a Panoptic ophthalmoscope while also minimizing the challenge and time required to manually align a lens, light source, and camera over a patient’s eye. Here, we report the development of our first generation, compact, user-friendly, attachment that mounts a typical condensing lens for indirect ophthalmoscopy to a smartphone. The device is a lightweight, 3D printed adapter that directly and reversibly couples iPhones 4 and higher to standard indirect ophthalmoscopy condensing lenses. The attachment is designed to hold a specific lens at a prescribed but adjustable distance from the camera lens, is easily assembled and disassembled (if desired), and can utilize either the phone’s native flash for lighting or another coaxial light source. With both mechanical prototypes and subsequent 3D printed versions of the device, we were able to quickly photodocument a variety of retinal pathologies.
Methods
We started with a computer aided design (CAD) model of a lens mount customized to the Panretinal 2.2 (Volk Optical, Inc. Montor, OH) condensing lens, with a slight undersized fit to allow gripping of the lens for easy insertion and removal. The mount was designed with the SpaceClaim 2012+ CAD package (SpaceClaim Corporation, Concord, MA). The initial 3D printed mount was manufactured on a desktop Rostock Max fused deposition modeling (FDM) 3D Printer (Open Source design by SeeMeCNC, Goshen, IN built by author AS in Stanford, CA). A mechanical prototype was then configured by screwing the 3D printed lens mount to the distal end of an assembly of digital SLR photography mounting accessories: a ball head camera mount with extender (Videosecu, Carrollton, TX), a mini ball head camera mount (Giottos, Pine Brook, NJ), and a universal smartphone tripod mount (Square Jellyfish, USA) (Figure 1a). A ray tracing of the optics of this lens adapter system, which is based on the optics of indirect ophthalmoscopy, is shown in Figure 1b.

Figure 1a: Mechanical prototype of lens-to-smartphone mount with 3D printed Panretinal 2.2 condensing lens holder
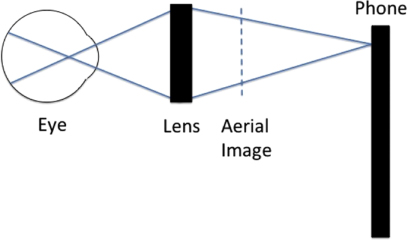
Figure 1b: Ray tracing (not to scale) of the optics of the lens adapter system
This prototype was then tested clinically to see if high quality images could be obtained and whether the alignment and working distances were correct. Once these were confirmed, another CAD iteration was made on SpaceClaim (Figure 2a). The full adapter design includes the lens mount, a smartphone adapter and a telescopic arm. This design was printed at the Stanford Product Realization Laboratory Room 36, using the 3D Systems (Rock Hill, SC) ProJet 3500 HD Multi-Jet Modeling (MJM) 3D Printer at a 32 micron resolution. VisiJet Crystal material (acrylic-like) was used for the part as well as wax support material, which was removed after a post processing step (wax melting and sonication) (Figure 2b). The mount (shown in Figure 2c) was designed to allow the user to hold the phone upright with one hand (Figure 2d) and to use the other hand to stabilize (if needed) but not actually hold the mounted lens over the patient’s eye.
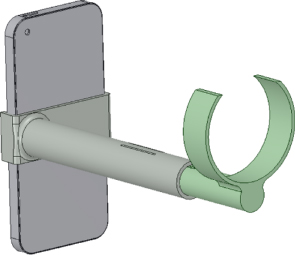
Figure 2a: CAD rendering of lens-to-smartphone mount
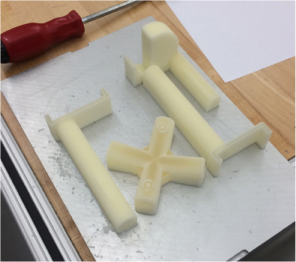
Figure 2b: Raw 3D printed lens mount with support material
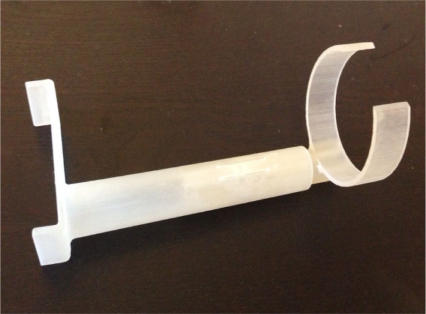
Figure 2c: 3D printed acrylic lens-to-smartphone mount based on CAD design in Figure 2a

Figure 2d: Volk Panretinal 2.2 indirect ophthalmoscopy condensing lens mounted to iPhone 5
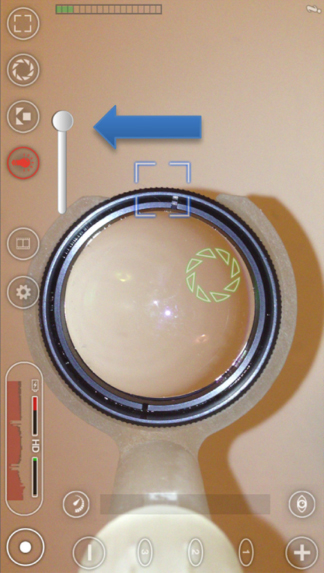
Figure 2e: Screenshot of adapter and condensing lens in place as imaged through the FilmicPro application with constant flash on lowest intensity indicated by the blue arrow
The Institutional Review Board at Stanford has approved the collection and analysis of fundus images using our system throughout the hospital (Protocol #25524). Smartphone fundus images were captured with an iPhone 5 (Apple Inc., Cupertino, CA, USA) a Panretinal 2.2 lens (Volk Optical Inc., Mentor, OH, USA), and our lens attachment in dilated patients. The iPhone’s native flash was used as a coaxial light source, and the acrylic, 3-D printed mount was used to create indirect ophthalmoscope system and capture digital images of the fundus with the smartphone camera [2]. Previously, Haddock et al.5 reported on the use of the iPhone application Filmic Pro (Cinegenix LLC, Seattle, WA, USA; http://filmicpro.com/) for fundus photography with a manually held condensing lens with and without a Koeppe lens5, and this application was used to provide constant adjusted illumination and video capture in conjunction with our adapter. The application’s video recording was activated, and a video of the fundus was captured on the iPhone screen. Once the areas of interest were filmed, the video library of the app was accessed and the recorded video was selected and exported to the camera roll. Still images were extracted from the video by screenshot. Videos were taken at 24 fps at 1080p resolution; for a typical 10 second capture, the files were approximately 50 MB in size. Screenshots were 1-2 MB at maximum resolution. However, we found that these files could be compressed upon transmission through secure email down to approximately 100 kB and still be adequate for clinical use.
For protection of privacy, photographs taken with these adapters are being transmitted either through secure, encrypted institutional email or through a HIPAA-compliant messaging application called Medigram (Los Altos, CA), which has been approved and is being deployed by the Stanford Hospital IT department for the capture and transmission of textpages and photos. All phones that are used to capture images are encrypted using the university or hospital Mobile Device Management (MDM) application. All image acquisition and transmittal was handled with strict attention to the confidentiality of personal data in accordance with the Data Protection Act of 1998 and Access to Health Records of 1990.
Results
Initially, fundus images were successfully captured on a model eye and subsequently in patients first using the mechanical prototype with 3D printed lens holder (shown in Figure 1). Subsequently, the fully 3D printed lens-to-phone attachment (Figure 2a–d) was used to photograph the retinas of patients with their permission. Samples of images captured by the mechanical prototype are shown in Figure 3a–c, while images captured by the 3D printed prototype are shown in Figure 4a–c.
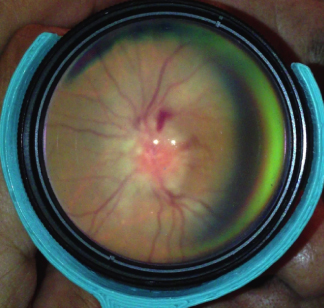
Figure 3a: Acute papillitis in a patient with ocular syphilis using the mechanical prototype adapter with 3D printed lens holder
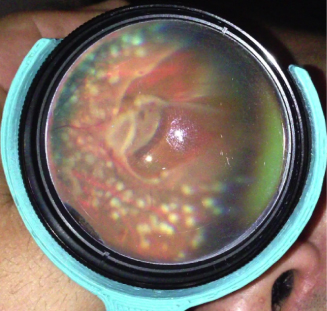
Figure 3b: Superior horseshoe retinal tear after laser retinopexy using the mechanical prototype adapter with 3D printed lens holder
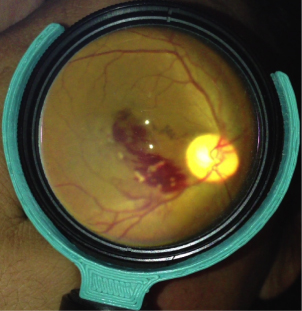
Figure 3c: Branch retinal vein occlusion using the mechanical prototype adapter with 3D printed lens holder
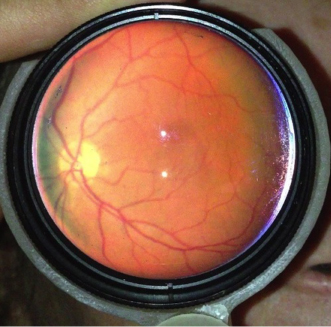
Figure 4a: Normal retina photographed using the fully 3-D printed lens-to-phone mount
The attachment as currently designed is lightweight, and only slightly longer (5.75 inches) than the length of an iPhone 5. There is a sliding shaft to enable adjustment of the working distance between the phone and the lens. Longer working distances were also possible but created problems with weight distribution and overall size/length issues with the device itself. This working distance was found to work well across patients, in spite of a range of axial lengths and levels of refractive error as the iPhone camera has an autofocus capability.
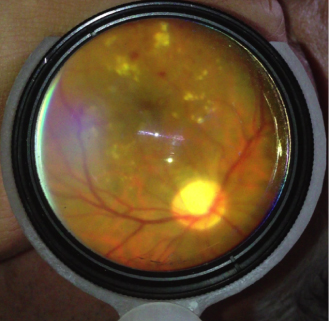
Figure 4b: Diabetic macular edema photographed using the fully 3-D printed lens-to-phone mount

Figure 4c: RPE hypertrophy photographed using the fully 3-D printed lens-to-phone mount
Figure 3a–c are examples of photos taken in the clinic of optic nerve swelling (Figure 3a), retinal horseshoe tear after indirect laser retinopexy (Figure 3b), and a branch retinal vein occlusion (Figure 3c) using the mechanical prototype with 3D printed lens holder.
Figure 4a–c are examples of photos taken in the clinic of normal and abnormal retinas taken with the fully 3D printed lens-to-phone mount. Figure 4a shows a normal fundus, Figure 4b shows a diabetic macular edema, and Figure 4c shows RPE hypertrophy.
Similar results have been achieved with mechanical prototypes mounted with other common ophthalmic lenses (Ocular Instruments, Inc, Bellvue, WA) 28D and 40D lens, which provide the ability to take photos of patients with smaller pupil sizes at shorter working distances between the condensing lens and camera lens (data not shown).
Safety:
Luxmeter measurements of the iPhone 5 flash dimmed with the Filmic Pro application and illuminated through the Panretinal 2.2 condensing lens were consistent with the findings of Kim et al. 8, who showed that the light levels were 150 times below the thermal hazard limit and 240 times below the photochemical hazard limit set by the International Organization for Standardization (ISO 15004-2.2) 9 and 10 times below the levels produced by the commercially available Keeler Vantage Plus LED indirect ophthalmoscope. The lowest intensity level using the app was always used, which we measured at approximately 800 lux through a Volk Panretinal 2.2 condensing lens using a commercial luxmeter (Mastech Professional Luxmeter Model Number LX1010B) standardized to a model eye (Western Surgical Specialties, Benicia, CA), so the level of light intensity and energy was always well below what was measured previously by Kim et al. We found that this flash setting was comparable to the illumination provided by a Heine Omega 500 indirect ophthalmoscope at mid-level intensity through the same condensing lens on the same model eye. Maximum flash intensity through the same lens/adapter/phone configuration to view a model eye was measured at about 2000 lux.
Discussion
Our case report demonstrates the proof of concept that high quality fundus images can be easily and reproducibly captured by the lens adapter described, coupled with an iPhone 5 and the Filmic Pro application. Haddock et. al. have published similar results while manually holding an indirect BIO lens with and without a Koeppe lens.5 Our design is believed to be an improvement for ease-of use as the adapter places the lens at an optimized position with respect to the camera’s field of view, minimizing time spent capturing the image.
In our design, we customized the attachment to be specific for holding a Volk Panretinal 2.2 lens on one side and an Apple iPhone 5 on the other. We determined that the ease of use of the device was greatly diminished when additional degrees of freedom were allowed between the lens and the smartphone camera and therefore concluded that fixed positions at all points was the optimal configuration. The autofocus capabilities of the iPhone were able to adjust for variations in patient refractive error. Although this particular adapter was customized to the dimensions of an iPhone, its design is readily modified to hold existing lenses of other dimensions and other models of smartphones. In addition to the Filmic Pro application, we used other commercially available applications such as CameraAwesome and ProCamera for identifying the area of interest and exposure. However, the light intensity was found to be too high from the native smartphone light source and so we needed to use either polarizing filters or neutral density filters to reduce the light intensity to tolerable levels for patients without degrading image quality. One incidental advantage that “video mode” (using FilmicPro or other applications) does provide over “camera mode” is a pre-set zoom that better fills the phone’s screen with the condensing lens held by the adapter; in camera mode, the user needs to apply a small amount of digital zoom to do so. Haddock et al. also described the use of either the app MovieToImage (DreamOnline, Inc., Tokyo, Japan; http://www.dreamonline.co.jp/) or Video 2 Photo (Francis Bonnin, PacoLabs; http://pacolabs.com/)5 that allowed the video clip still-image extraction but these software apps were not used in this study.
Of note, the Filmic Pro application only allows for video capture in conjunction with variable LED functionality and as a result, file size and storage becomes a problem. The method describe herein of taking screenshots of paused video is less than ideal, both from a workflow and image resolution perspective. The Welch Allyn iExaminer application does capture multiple selectable frames rather than a straight video, but does not provide control over the flash. As a remedy to this, we are developing a modification to the adapter that includes a co-axial, variable intensity, external LED light source that obviates the need for the phone’s native flash. This frees the adapter from the FilmicPro application and allows capture of the highest resolution images using the phone’s stock camera or with the camera functions of other HIPAA-compliant image-transfer applications, such as EPIC Haiku. In addition, it would make the adapter “agnostic” to not only the type of application used, but also the type of phone used, since every phone has a slightly different alignment of flash and camera lens, and not every phone and platform has an application that can control LED intensity. This is especially important as the smartphone landscape continues to rapidly evolve.
Conclusions
The tools of secure message transmission, smartphones with cloud access and high quality camera technology, and a user-friendly, low cost adapter to easily couple lenses to a smartphone are now making teleophthalmology increasingly accessible. Our team is currently studying the concordance between remote clinical decisions made from viewing these retinal images compared to information gleaned from a standard eye examination through an IRB-approved study at Stanford Hospital. In this same study, photo quality is being evaluated by a panel of faculty reviewers. Our ultimate goal is for this system to be usable by healthcare staff with minimal specialized training to remotely capture and share high quality retinal images in order to enhance healthcare provider communication. An example would be enabling a triage nurse to text a secure, reliable image to an ophthalmologist on-call. In future work, we plan to deploy subsequent generations of the adapter to non-ophthalmologists to determine the efficacy of smartphone-based photography for remotely triaging patients when access to an ophthalmologist is limited.
Disclosure
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf and declare: a patent pending on the submitted work but no support from any organisation for the submitted work and no financial relationships with any organisations that might have an interest in the submitted work.
Acknowledgements
The authors would like to thank the faculty and staff at the Stanford Product Realization Laboratory for their support of the 3D printing work presented in this paper.
References
1. Hester C. Available at: http://eyewiki.aao.org/Smart_Phoneography_-_How_to_take_slit_lamp_photogra phs_with_an_iPhone.
2. Teichman JC, Sher JH, Ahmed IIK. From iPhone to eyePhone: A technique for photodocumentation. Canadian Journal of Ophthalmology/Journal Canadien d’Ophtalmologie 2011;46(3):284–6.![]()
3. Lord RK, Shah VA, San Filippo AN, Krishna R. Novel uses of smartphones in ophthalmology. Ophthalmology 2010;117(6):1274. e3. ![]()
4. Chakrabarti D. Application of mobile technology in ophthalmology to meet the demands of low-resource settings. Journal of Mobile Technology in Medicine 2012;1(4S):1–3. ![]()
5. Haddock LJ, Kim DY, Mukai S. Simple, Inexpensive Technique for High-Quality Smartphone Fundus Photography in Human and Animal Eyes. Journal of Ophthalmology 2013;2013. ![]()
6. Bastawrous A. Smartphone fundoscopy. Ophthalmology 2012;119(2):432–3. e2. ![]()
7. Chhablani J, Kaja S, Shah VA. Smartphones in ophthalmology. Indian J Ophthalmol 2012;60(2):127. ![]()
8. Kim DY, Delori F, Mukai S. Smartphone photography safety. Ophthalmology 2012;119(10):2200–1.![]()
9. International Standard I, 15004-2.2. Ophthalmic Instruments, Light Hazard Protection, 2007.

