Resident Impressions of the Clinical Utility and Educational Value of the iPad
Matthew Skomorowski, MD1, Kim Jordan, MD, FACP1, Kevin Schroeder, MD1, John O. Elliott, PhD, MPH1
1Department of Medical Education, Riverside Methodist Hospital, Columbus, USA
Corresponding Author: mskomor2@ohiohealth.com
Journal MTM 2:3:21–26, 2013
Background Physician use of the iPad as a clinical and educational tool has increased since its release in 2010. Few studies have assessed resident perception of the iPad as an educational and daily clinical tool.
Aims This study evaluates residents’ perceptions of the iPad’s clinical and educational utility, and examines differences of perceived value between medicine-based and surgical-based residents.
Methods During the academic year 2011–2012, all residents (n = 119) utilized a 16GB iPad. Opinions on clinical utility and educational value were assessed by survey at year’s end. Responses were dichotomized as often /always vs. never/rarely/sometimes for comparison analysis via Chi-square tests.
Results One-hundred-and-two (86%) residents participated. The iPad received low marks for daily clinical utility (14.7%) and efficiency in documentation (7.8%). It was most valued for sourcing articles outside the hospital (57.8%), and as a research tool (52%). Medical and surgical residents’ opinions differed regarding perceived value for educational utility (41.7% vs. 6.7%, p ≤ 0.001), viewing results and use as an Evidence-based Medicine resource (38.9% vs. 16.7%, p = 0.037), recommendation to a colleague (58.3% vs. 36.7%, p = 0.053), and facilitation of patient care (45.8% vs. 23.3%, p = 0.045).
Conclusion Residents in this study did not attribute high value to the iPad as a clinical rounding or educational tool. Additionally significant differences existed between medical and surgical residents’ perceived value of the iPad’s utility. Institutions should consider these differences and address connectivity and support issues before implementing iPad programs across all disciplines.
Introduction
The use of hand held computers by medical trainees isn’t new. A review published in 2006 found that 60 to 70% of medical students and residents were using hand held computers for educational purposes or patient care. The most commonly accessed applications included medical reference tools, electronic textbooks, and clinical computational programs.1 A review in 2009 found 90% of residents with personal digital assistants (PDAs) accessed pharmacological prescribing programs and medical calculators on a daily basis.2 Time management was dramatically improved for house staff who relied on PDAs for laboratory data retrieval.2
Since the iPad release in 2010, two independent market research studies have evaluated digital trends in medicine. In 2011, the Manhattan Research group reported that 81% of U.S. physicians own a smart phone, 30% were using an iPad, and 28% planned to purchase an iPad within six months.3 In 2012, Epocrates Research group found 34% of physicians used a tablet computer and 75% planned to buy one within a year. Eighty-one percent with a tablet also owned an iPad.4 However, iPad users reported that the onscreen keyboard was hard to use and use of a separate keyboard was self-defeating. Compatibility issues with the iPad were also problematic.5
There are emerging trends toward paperless iPad based curriculums at several medical institutions. A 2011 Yale School of Medicine initiative began as a way to reduce expenses and save paper, but also served to provide an enhanced student learning experience.6 Other universities have followed suit and report that introduction of iPad programs contributes to improved working conditions, patient care, and student education.7
In the current era of compressed duty hours and increased hand-offs, the iPad has the potential to improve resident efficiency and improve continuity of care. Few studies have assessed resident perception of iPad utilization and its’ benefit as both an educational and daily clinical tool. Patel et.al reported improvement in both perceived and actual resident efficiency in an Internal Medicine residency with implementation of the iPad.8 The authors noted that iPad use may have improved continuity of care, finding more orders were placed by the admitting team prior to rounds and departure of the post-call team.8 Studies of newly implemented iPad programs in select subspecialties of radiology and neurosurgery concluded that the iPad is a valuable educational tool, but did not assess clinical utility.9–12 Several other studies routinely focused on tablet or smart phone applications available to particular groups.13–17
This study’s aims were to assess resident perception of the iPad’s clinical and educational utility and to determine if differences of perceived value existed between medicine-based (Internal Medicine, Family Practice, Preliminary Medicine/Transitional year) and surgical/obstetrics and gynecology (General Surgery/Ob-Gyn) residents. Additionally, this study garnered information about the most useful and popular applications, and comments or ideas for improvement concerning iPad use. We hypothesized that our residents, overall, would rate the iPad as a useful tool for both daily clinical work and educational support.
Methods
In our hospital, orders are written on a paper based chart, otherwise workflow is electronic/computer based. Recognizing the emerging use of mobile electronic devices, Riverside Methodist Hospital initiated a resident-wide iPad program in the academic year 2011–2012. A small feasibility study with nineteen surgical residents was completed prior to residency-wide implementation of the iPad program to ensure successful access to the hospital’s electronic health record via VMware View Client, accessed via Wi-Fi.
A 16 GB iPad™ 2 with Wi-Fi at a cost of $499 each was utilized by each resident along with a $100 stipend to purchase auxiliary equipment such as case covers and keyboards. After a comprehensive orientation that included directions for accessing the hospital’s medical records, residents were instructed to use their iPad both in and outside the hospital as they saw fit throughout the year. White coats were fitted with an oversize pocket to effectively house the iPad.
Residents’ perceptions of the clinical and educational utility of the iPad were measured via an electronic survey completed at the end of the academic year. Questions were structured on a 5-point Likert scale (1 = never, 2 = rarely, 3 = sometimes, 4 = often, and 5 = always). In order to address the non-normality of ordinal data as well as to address different sample sizes in the medicine-based and surgical/obstetrics & gynecology groups based on our resident complement, the Likert scale was dichotomized as often/always = 1 and never/rarely/sometimes = 0 for comparison analyses via the Chi-square tests. A p-value of ≤ 0.05 was used to indicate statistical significance. Reliability statistics of the survey revealed strong internal consistency, Cronbach’s alpha = 91.5 (95% CI: 88.8-93.8). All analyses were conducted with IBM SPSS version 19.0.
Two questions allowed residents to list useful applications and provide general comments. These were summarized via descriptive statistics. One-hundred and nineteen residents in all levels of training (PGY-1 through PGY-5) and across all residencies (Internal Medicine, Family Practice, Preliminary Medicine & Transitional Year, General Surgery and Ob-Gyn) were invited to participate. The study was approved by the Institutional Review Board.
Results
One-hundred-and-two (86%) of 119 residents completed the survey. Across all residency programs, the iPad received low marks for clinical utility, described as use on rounds (14.7%) and efficiency in writing progress notes (7.8%). The iPad received its highest marks for educational value in terms of sourcing articles and researching topics outside of the hospital (57.8%). Fifty-two % of residents would recommend the iPad as a valuable research tool, see Table 1.
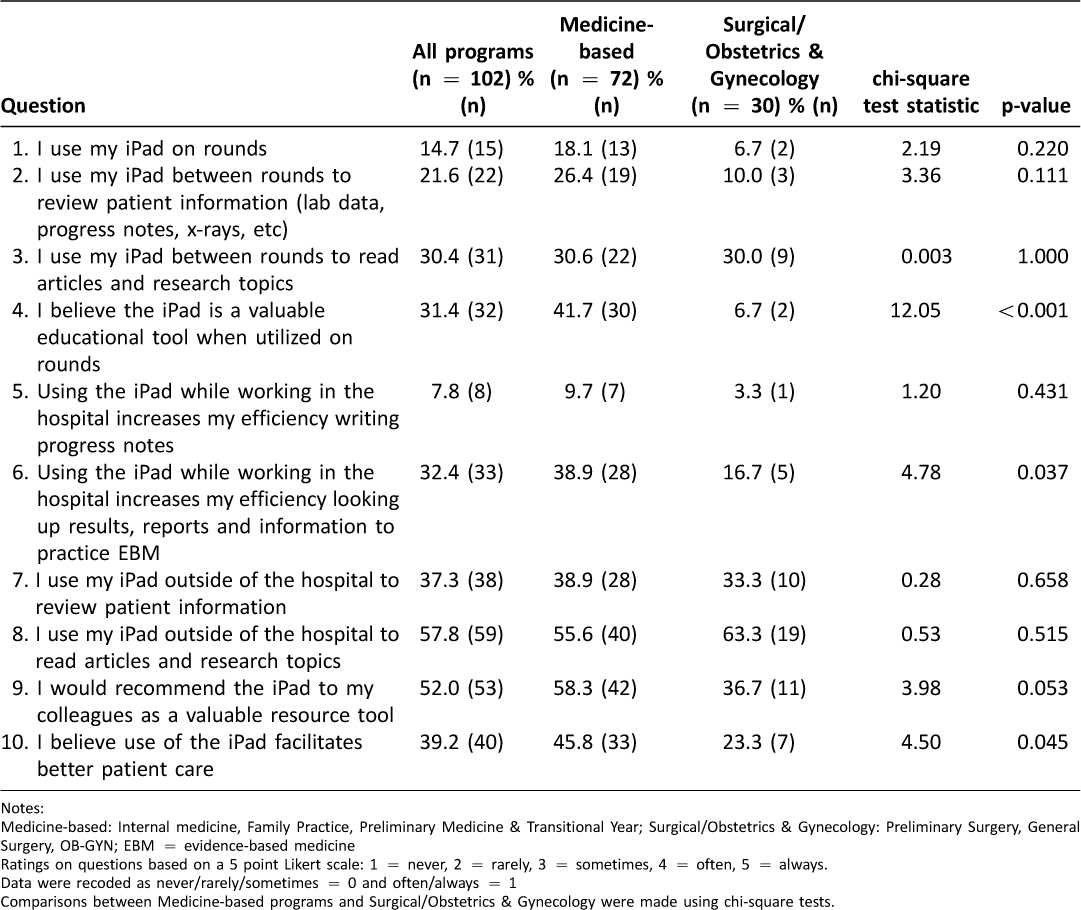 Table 1: Overall and by program, resident ratings of the iPad (% reporting often/always)
Table 1: Overall and by program, resident ratings of the iPad (% reporting often/always)
There was a significant difference in residents who reported often/always between the medicine-based and surgical/Ob-Gyn groups in terms of: the iPad as a valuable educational tool (41.7% vs. 6.7%, p ≤ 0.001), viewing results and as an Evidence-based Medicine (EBM) resource (38.9% vs. 16.7%, p = 0.037) and belief that the iPad facilitates better patient care (45.8% vs. 23.3%, p = 0.045). Additionally, medicine-based residents were more likely to recommend the iPad as a valuable resource to colleagues (58.3% vs. 36.7%, p = 0.053), see Table 1.
All resident groups noted problems with iPad log-in and connectivity/WiFi (40%). During the academic year 98 tickets specific for iPad set-up and connectivity issues were reported to Information Technology services (out of 182,000 global tickets). Additionally, all resident groups reported problems with utilization of the iPad for medical documentation/progress notes (12%). Portability (5%) and software applications (2%) were less problematic, see Table 2.
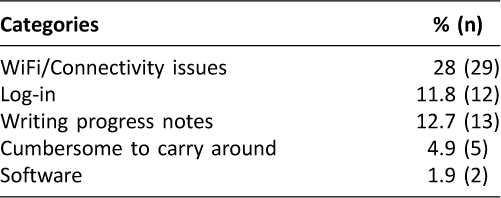
Table 2: General comments about problems with the iPad
The most frequently recommended iPad applications were medical tools such as ePocrates, Micromedex and EBM resources (Medscape and Uptodate). Other suggested applications included medication reference software. The single most frequently cited application was Riverside’s electronic medical record, see Table 3.
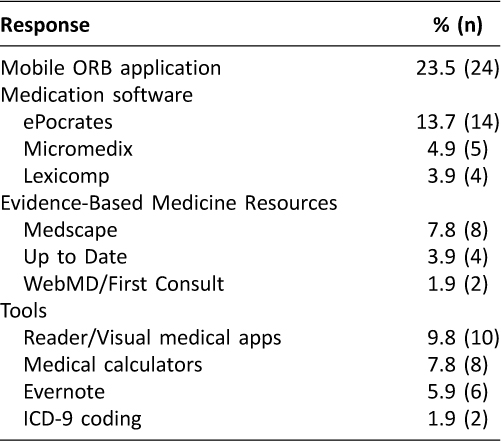
Table 3: Suggested programs/apps for the iPad (n = 102)
Discussion
Our study supports decreased utility of the iPad, particularly among non-medicine-based residents. We found that residents across all disciplines did not perceive the iPad to be clinically useful on daily work rounds, and had only slightly increased value as an educational tool.
In this study, medicine-based residents were more likely to report that the iPad was a valuable educational tool when utilized on rounds than did their surgical/Ob-Gyn counterparts. Though not addressed by this study, disparity may exist due to differences in clinical rounding styles as well as the working life of medical vs. procedural-based residents with different emphasis on data use and interpretation. For example, at our institution, medical residents receive weekly conferences in an evidence-based medicine curriculum, and are expected to employ a consistent evidence-based approach to decision-making during clinical rounds; thus, they may perceive the iPad to be a more useful educational tool (sourcing articles, accessing data) during clinical rounds than do procedural-based residents.
Our study suggests that resident efficiency may be less positively impacted by use of the iPad than previously reported.8 On the iPad, our EHR is accessed via remote desktop, requiring a two-step login process. Though log-in and connectivity issues were noted as a significant problem, technology support was rarely utilized. Residents often found it faster to use a computer than reporting difficulties. Additionally, electronic order entry is not available at our hospital. Consequently, workflow on the iPad was disjointed; residents were unable to do everything in one place (view results, place orders and/or document) which may have negatively affected efficiency and perception when using the iPad on daily rounds (see sample comments in Table 4).
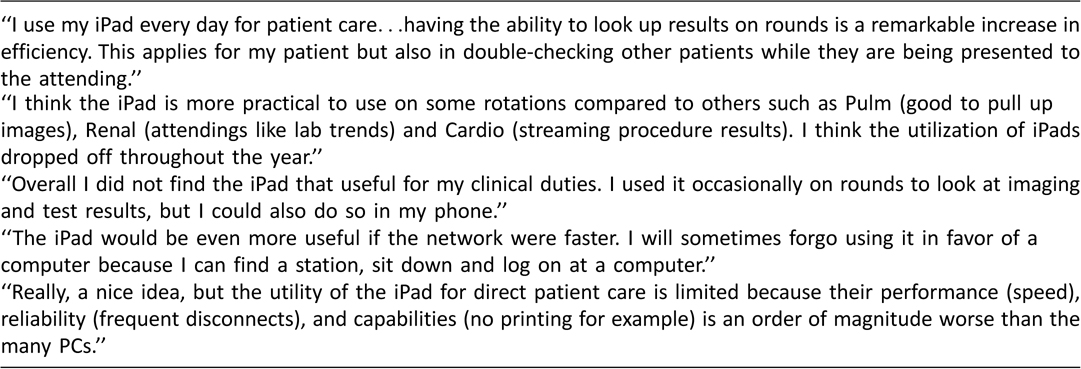 Table 4: Sample individual resident comments
Table 4: Sample individual resident comments
Studies evaluating the use of the iPad as an educational tool have reported mixed results. While Patel et al. described improved resident efficiency with iPad use, recent reports note mixed results on the utility of the iPad in a medical setting and that iPad use as been less pronounced in clinical workflow than earlier studies indicate.8, 18 Additionally, satisfaction or use of the iPad may decline after its initial implementation in both educational and clinical settings.19, 20
Limitations to this study exist. This study was a single institution study; therefore its findings may be unique. Recall bias may also be a limiting factor as we did not track or measure actual use of the iPad and results are solely predicated on opinions. Low rating of medical apps may be more reflective of lack of quality and quantity available in the market at the time of the study. Although a small pilot was performed, connectivity issues were not fully addressed prior to implementation of the program – which may have limited use; higher usage may have resulted in improved ratings. Additionally, “tech savvyness” was not rated; information was not collected on prior use or actual hours of iPad use by all residents. Finally, this study was created de novo and reliability testing showed strong internal consistency between responses. However, validity testing was not performed. It is understood the best objective validity test would have been a measure of actual iPad use. Our survey had a high response rate and is one of the first to make comparisons in educational and clinical utility across several medical disciplines.
Conclusion
Utilization of mobile technology in medical education and residency programs continues to expand. This study found significant differences between medical and surgical residents’ perceived value of the iPad’s utility as both an educational and clinical rounding tool. Further exploration of these differences may warrant consideration by institutions planning to implement iPad programs across all disciplines. Additionally, factors such as hardware/software cost, vendor support, on-going training, in-house support, and connectivity should be considered prior to implementation of a mobile computing program. The availability and utilization of mobile technology continues to grow at a rapid pace. Further study is required to both monitor and measure its impact on improving the educational and clinical goals of medicine.
References
1. Kho A, Henderson LE, Dressler DD, Kripalani S. Use of handheld computers in medical education – A systematic review. J Gen Intern Med. 2006;21:531–7. ![]()
2. Tempelhof MW. Personal Digital Assistants: A review of current and potential utilization among medical residents. Teaching and Learning in Medicine. 2009;21:100–4. ![]()
3. Manhattan Research. 75 Percent of U.S Physicians own some form of Apple device. Available at: http://manhattanresearch.com/News-and-Events/Press-Releases/physician-iphone-ipad-adoption. Accessed January 15, 2013.
4. Chang MA. Epocrates Mobile Trends Report: Rise of the Digital Omnivore, M.D. Epocrates. June 2012;5–9.
5. Katz PS. Mobile devices offer advantages, challenges. ACP Internist. 2012;32.
6. Dodson H. Going green and digital: iPads for all at Yale school of medicine. Yale News. Aug 23, 2011. Available at: http://news.yale.edu/2011/08/23/goinggreen-and-digital-ipads-all-yale-school-medicine-0. Accessed August 5, 2012.
7. Pickert Kate. IPAD, M.D. Time. 2012;55.
8. Patel BK, Chapman CG, Luo N, Woodruff JN, Arora VM. Impact of mobile tablet computers on internal medicine resident efficiency. Arch Intern Med. 2012;172:436–7. ![]()
9. Korbage AC, Bedi HS. Mobile Technology in Radiology Resident Education. J Am Coll Radio. 2012;9:426–9. ![]()
10. Tanaka PP, Hawrylyshyn KA, Macario A. Use of table (iPad) as a Tool for Teaching Anesthesiology in an Orthopedic Rotation. Revista Brasileria de Anestesiologia 2012;62:214–22.
11. Davis JS, Garcia GD, Wyckoff MM, et al. Use of mobile learning module improves skills in chest tube insertion. J Surg Res. 2012;177(1):21–6. ![]()
12. Gonzalez NR, Dusick JR, Martin NA. Effects of Mobile and Digital Support for a Structured, Competency-Based Curriculum in Neurosurgery Residency Education. Neurosurgery 2012;71(1):164–72. ![]()
13. Goff DA. iPhones, iPads, and Medical Applications for Antimicrobial Stewardship. Pharmacotherapy 2012;32(7):657–61. ![]()
14. Franko O, Tirrel T. Smartphone App Use Among Medical Providers in ACGME Training Programs. J Med Syst 2012;(36):3135–9. ![]()
15. Franko OI, Bhola S. iPad Apps for Orthopedic Surgeons. Orthopedics 201;34(12):978–81.
16. Kiser K. The iPad Project. Minn Med 2011;94(4):12–4.
17. Rohrich RJ, Sullivan D, Tynan E, Abramson K. Introducing the New PRS iPad App: The New World of Plastic Surgery Education. Plast Reconstr Surg 2011 Sep;128(3):799–02. ![]()
18. Luo N, Chapman CG, Patel BK, et al. Expectations of iPad use in an internal medicine residency program: is it worth the “hype”? J Med Internet Res. 2013 May 8;15(5):e88. ![]()
19. Berkowitz SJ, Kung JW, Eisenberg RL, et al. Resident iPad Use: Has It Really Changed the Game? J Am Coll Radiol. 2013 Jun 25. pii: S1546-1440(13):271–8. ![]()
20. George P, Dumenco L, Doyle R, et al. Incorporating iPads into a preclinical curriculum: a pilot study. Med Teach. 2013;35(3):226–30. ![]()

