Patient-oriented Health Technologies: Patients’ Perspectives and Use
Patient-oriented Health Technologies: Patients’ Perspectives and Use
Amy M. Bauer, MD, MS1*, Tessa Rue, PhD2,3, Sean A. Munson, PhD4, Reza Hosseini Ghomi, MD, MSE1, Gina A. Keppel, MPH3,5, Allison M. Cole, MD, MPH3,5, Laura-Mae Baldwin, MD5, Wayne Katon, MD1
1Psychiatry and Behavioral Sciences, University of Washington, Seattle, USA; 2Biostatistics, University of Washington, Seattle, USA; 3Institute of Translational Health Sciences, University of Washington, Seattle, USA; 4Human Centered Design & Engineering, University of Washington, Seattle, USA; 5Family Medicine, University of Washington, Seattle, USA
*Dr. Bauer is the recipient of an NIH-funded Career Development award through the Institute of Translational Health Sciences at University of Washington.
Corresponding Author: abauer1@uw.edu
Note: This manuscript includes data that has been presented at the 2015 Translational Science annual meeting.
Journal MTM 6:2:1–10, 2017
Background: For patient-oriented mobile health tools to contribute meaningfully to improving healthcare delivery, widespread acceptance and use of such tools by patients are critical. However, little is known about patients’ attitudes toward using health technology and their willingness to share health data with providers.
Aims: To investigate primary care patients’ comfort sharing health information through mobile devices, and patients’ awareness and use of patient portals.
Methods: Patients (n=918) who visited one of 6 primary care clinics in the Northwest US completed a survey about health technology use, medical conditions, and demographics.
Results: More patients were comfortable sharing mobile health information with providers than having third parties store their information (62% vs 30%, Somers D=.33, p<0.001). Patients older than 55 years were less likely to be comfortable sharing with providers (AORs 0.37-0.42, p<0.01). Only 39% of patients knew if their clinic offered a patient portal; however, of these, 67% used it. Health literacy limitations were associated with lower portal awareness (AOR=0.55, p=0.005) but not use. Portal use was higher among patients with a chronic condition (AOR=3.18, p=0.004).
Conclusion: Comfort, awareness, and use of health technologies were variable. Practices introducing patient-facing health technologies should promote awareness, address concerns about data security, and provide education and training, especially to older adults and those with health literacy limitations. Patient-facing health technologies provide an opportunity for delivering scalable health education and self-management support, particularly for patients with chronic conditions who are already using patient portals.
Introduction
The potential for health information technologies (HIT) to play a transformative role in health service delivery has received considerable recent attention, with much enthusiasm focused on how patient-oriented technologies can improve care for chronic medical and behavioral health conditions.1,2 Such technologies include electronic patient portals, mobile health smartphone applications (apps), wearable biosensors, and other home-based systems allowing the collection, display, and transmission of patient-generated health data.3 Because smartphone adoption has been disproportionately high amongst racial and ethnic minorities,4 mobile health technologies may reach segments of the population that have been historically underserved in healthcare settings, thus representing a potential opportunity to address healthcare disparities for certain groups. The rapid growth of the consumer mobile health market into a multibillion dollar industry reveals strong consumer interest in using mobile health tools and recent industry reports suggest high levels of consumer trust in mobile health technologies.5,6 However, for patient-oriented technologies to have a substantial impact on the delivery of healthcare, it would be necessary for these tools to enable the straightforward transmission of patient-generated health data to healthcare providers, and it is unclear whether consumer interest and trust extend to such tools that facilitate data-sharing.
In contrast to the consumer market, the healthcare sector has been slow to adopt information technologies, and using such technologies to engage patients is a recent innovation. In 2008, less than 10% of hospital systems in the United States had any electronic medical record system, and by 2013 only 6% met Stage 2 Meaningful Use criteria, which include a basic patient portal.7,8 Privacy concerns and security breaches involving health information may present barriers to patient adoption of mobile health tools that communicate directly with healthcare providers or may discourage their disclosure of sensitive information.9,10 Furthermore, early reports have identified disparities in patients’ use of portals associated with sociodemographic characteristics including race/ethnicity and health literacy.11–14
For patient-oriented mobile health tools to contribute meaningfully to improvements in healthcare delivery by facilitating patient education and engagement or enhancing patient-provider communication, widespread acceptance and use of such tools by patients are critical. However, little is known about patients’ attitudes toward using health technology and their willingness to share health data with providers. To address this gap in knowledge, this study aimed to assess the perspectives of primary care patients in community-based clinics in a practice-based research network in the 5-state WWAMI (Washington, Wyoming, Alaska, Montana, Idaho) region on the use of patient-oriented health technologies. We evaluated patients’ comfort using mobile health tools to share health information and their awareness of and use of patient health portals, hypothesizing that patients would be more comfortable sharing mobile health data with their healthcare providers than with third parties (i.e., companies that are not a part of the provider system). In addition, we examined demographic and clinical correlates of comfort, awareness, and use.
Methods
Study Sites
Study sites were six primary care clinics within the WWAMI region Practice and Research Network (WPRN) that chose to participate because they were interested in mobile health. Several sites had participated in a separate study with similar methods immediately prior to the current study. Participating clinics were located in four states (Washington, Wyoming, Alaska, Idaho) and included four hospital-associated outpatient practices, one office practice, and one Federally-Qualified Health Center. At the time of the study, five of the sites had an online patient portal available for patients. The clinics serve many low-income patients (22%-62% of patients uninsured or receiving Medicaid). Participating sites received an administrative stipend of $500. At each site, a champion was engaged throughout the project to assist in study design, coordination, and implementation.
Participants and Procedures
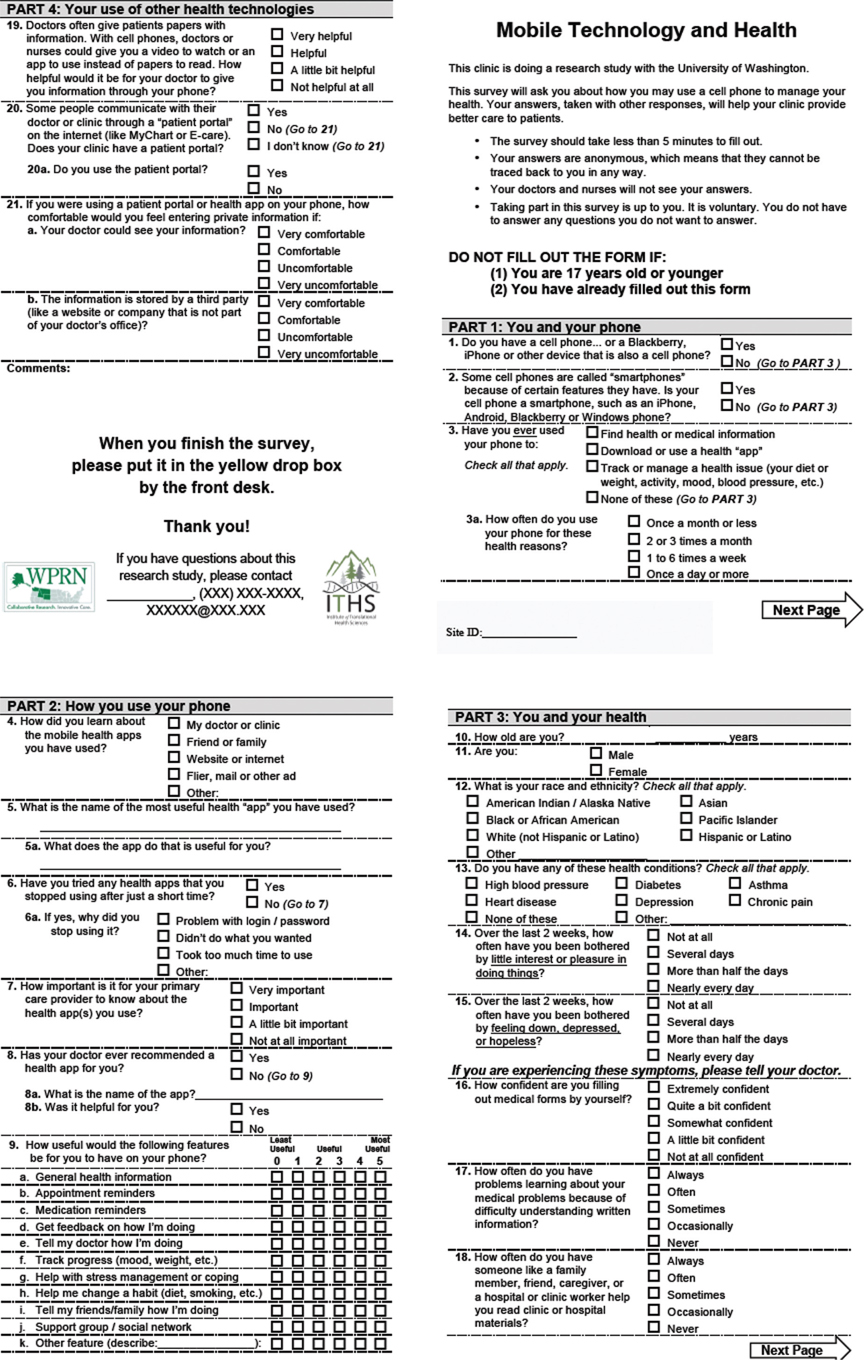
All adult patients (ages 18 and over) seen for a visit in any of the participating sites during a 2-week period in June 2013 were given a brief questionnaire (see Appendix) when they checked in for their appointment.15 The anonymous survey was designed to be completed in less than 5 minutes and returned to a collection box in the waiting area. Patients were informed that participation was voluntary and would not affect their healthcare. The surveys had unique tracking numbers used to facilitate estimation of the response rate. This study was considered minimal risk and was granted an exempt determination by the Institutional Review Board at the University of Washington. Additional details of the sample and methods have been reported previously.16
Measures
Participants reported their age, gender, self-reported ethnicity, and completed a 3-item measure of health literacy that has been validated in a variety of medical settings.17–19 Consistent with prior research, scores from each item were summed to yield a total score from 3 (poor health literacy) to 15 (no health literacy limitations) and coded dichotomously as having any health literacy limitation (scores 3–14) versus none (score=15).11,20 As much of the enthusiasm for mobile health tools centers on their potential role for managing chronic medical and behavioral health conditions, participants were asked to report on depressive symptoms and the presence of chronic medical conditions. Participants completed the 2-item Patient Health Questionnaire (PHQ-2), a validated measure of depressive symptoms, scored from 0 to 6, with a cutpoint of 3 to identify patients with probable major depression.21,22 Participants also reported whether they had a history of depression or any of the following common chronic medical conditions: high blood pressure, diabetes, heart disease, asthma, chronic pain, or any other chronic condition not listed.
Mobile phone ownership and mobile health use
Mobile and smartphone ownership were assessed by two questions adapted from the Pew Internet & American Life project.23 Mobile health use was assessed by asking participants if they have ever used their phone to “find health or medical information”; “download or use a health ‘app’”; or “track or manage a health issue (your diet or weight, activity, mood, blood pressure, etc.)”.
Attitudes about mobile health data-sharing
Comfort with sharing mobile health data was assessed by asking participants “if you were using a patient portal or health app on your phone, how comfortable would you feel entering private information if (a) your doctor could see your information; (b) the information is stored by a third party (like a website or company that is not part of your doctor’s office)”. Responses were coded as “very comfortable”/“comfortable” versus “uncomfortable”/“very uncomfortable”.
Patient portal awareness
Participants reported whether their doctor or clinic has a patient portal (like MyChart or E-care) for patients to communicate with their doctor or clinic, with responses “yes”, “no,” and “I don’t know”.
Patient portal use
Participants who reported that their clinic has a patient portal were asked whether or not they use the patient portal.
Data Analysis
Data from the surveys are stored electronically on a secure server at the University of Washington. Because the survey was anonymous, no identifying information is contained in the data files. Descriptive statistics were used to characterize attitudes about mobile health data-sharing, patient portal knowledge and use. To assess whether attitudes differed for sharing mobile health data with providers versus third parties, a significance test of Somer’s D was performed. This Somer’s D statistic tested for the difference in proportion endorsing comfort sharing data with provider versus comfort sharing data with a third party accounting for person-level and site-level clustering of responses. To examine correlates of patients’ attitudes about mobile health data-sharing, separate mixed effects logistic regression models estimated the adjusted associations between patient characteristics (age, gender, race/ethnicity, health literacy, chronic conditions, and depression) and attitudes. Separate models were constructed for each item (comfort sharing with a healthcare provider and comfort with third-party storage). To the fully adjusted models, we assessed the associations between attitudes and mobile phone ownership by adding a term for mobile phone ownership. To assess the additional associations of attitudes with smartphone ownership and mobile health use, we conducted analyses on a subset of the patients. First, among patients who own mobile phones, we assessed the association between attitudes and smartphone ownership by constructing fully adjusted mixed effects logistic regression models with a term for smartphone ownership. Finally, among patients who own smartphones, we assessed the association between attitudes and mobile health use by constructing fully adjusted mixed effects logistic regression models with a term for mobile health use. For each of these analyses, separate models were constructed for each dependent variable (comfort sharing with a healthcare provider and comfort with third-party storage). Similarly, separate models were constructed to assess correlates of patient portal awareness and patient portal use in a subset of the sample. Patients treated in the one clinic that did not offer a patient portal at the time of the study were excluded from both models. The model assessing portal use was restricted to only patients who endorsed awareness of their clinics’ portal. Multiple imputation (m=40) was used to impute missing independent variables in multivariate models using Stata’s “mi” commands. All variables were included in the imputation and assumed to have a multivariate normal distribution. Multivariate regressions were performed on each imputed data set and results combined using Rubin’s rules.24
Results
As reported previously, 918 participants completed the survey for an estimated response rate of 67.4%.16 As is typical of primary care patients, a majority of participants were female (75%), and many had health literacy limitations (62%), chronic medical conditions (63%), and current depressive symptoms (21%). Participants spanned a range of ages (range: 18-94 years; 15% 18-24 years, 21% 25-34 years, 19% 35-44 years, 19% 45-54 years, 16% 55-64 years, 9% 65 years or greater; mean=42.7 years; SD=15.9 years) and ethnicities (80% non-Hispanic white, 5% Hispanic or Latino, 4% Asian American/Pacific Islander, 2% African American, 9% American Indian/Alaska Native or multiracial/other).
Attitudes about mobile health data-sharing
Among 789 participants who responded to the survey items assessing attitudes about data-sharing, a majority (62%, n=493) were comfortable or very comfortable sharing data with their healthcare provider, but most (70%, n=550) were uncomfortable or very uncomfortable with third-party storage of mobile health data, a difference that is statistically significant (Somers D=.33, p<0.001). Patients above the age of 55 years were significantly less likely to report comfort sharing mobile health data with providers than counterparts under 25 years (AORs 0.37-0.42, p<0.01), whereas gender, race/ethnicity, health literacy, chronic conditions and depressive symptoms were not significantly associated with comfort (Table 1). In contrast, comfort with third-party storage of mobile health data was unrelated to patient characteristics (Table 1). Technology ownership and use were significantly associated with attitudes toward mobile health data-sharing. Specifically, mobile and smartphone ownership and mobile health use were each significantly associated with greater comfort sharing mobile health data with healthcare providers (AORs 1.77-3.04, p<0.01), with similar but less pronounced patterns evident for comfort with third-party storage (Table 2). After accounting for mobile or smartphone ownership, the association between age and comfort sharing mobile health data with providers was unchanged (AORs 0.38-0.46, p<0.05), however this association was attenuated in the model that included mobile health use (Age 55-64 years: AOR=0.68, NS; Age>65 years AOR=1.85, NS; data not shown in Table).
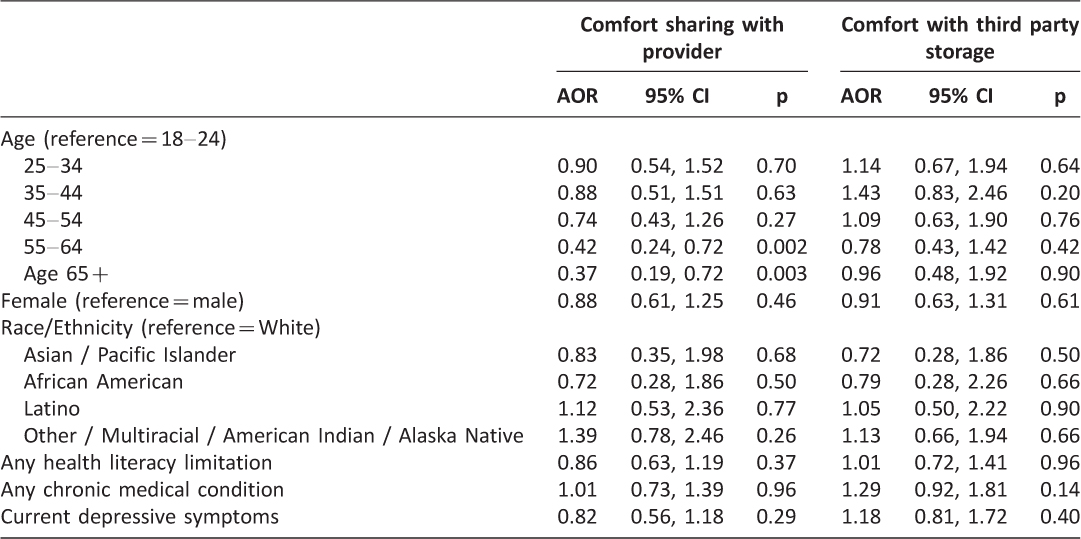
Table 1: Associations between patient characteristics and attitudes about mobile health data-sharing. (n=789)
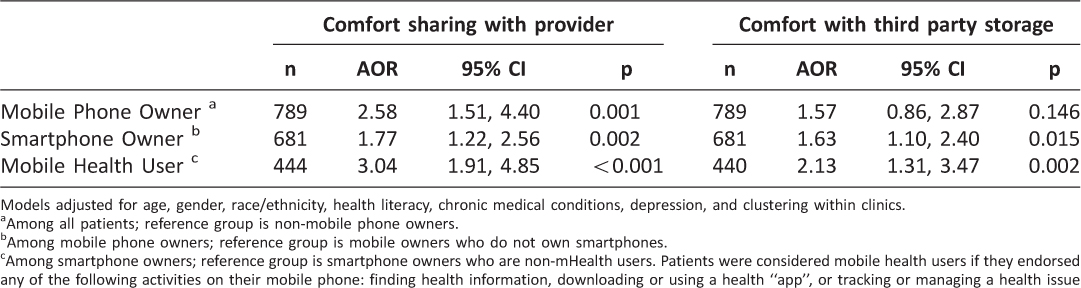
Table 2: Associations between mobile technology ownership and use and attitudes about mobile health data-sharing.
Patient portal awareness
Among 815 participants who responded to questions about the patient portal, most did not know whether their clinic had an electronic patient portal (53%, n=433) or responded incorrectly to the survey item (8%, n=67). Specifically, 59 patients (12%) from the 5 clinics with a patient portal indicated that the clinic did not have a portal and 8 patients (2%) at the clinic without a portal reported that their clinic did have one. Among 481 participants from the 5 clinics with portals, patients with any health literacy limitations were significantly less likely to know about the portal than counterparts without health literacy limitations (AOR=0.55, p=0.005), whereas patient demographic variables, chronic medical conditions, and depressive symptoms were unrelated to awareness of the patient portal (Table 3).
Patient portal use
Among 186 participants who knew about the patient portal at the 5 clinics with one, two-thirds (67%, n=125) reported that they had used the portal. Patients with chronic medical conditions were significantly more likely than healthy counterparts to use the portal (AOR=3.18, p=0.004; Table 3) and individuals ages 25 to 44 years were somewhat more likely to use the portal than counterparts between 18 and 24 years of age (AORs 2.94-2.95, p<0.10). Gender, race/ethnicity, health literacy, and current depressive symptoms were unrelated to use of the patient portal among patients who knew about it. In addition, patients’ report of their comfort sharing mobile health data with providers was strongly associated with use of the patient portal (AOR=3.67, 95% CI 1.66-8.13, p=0.001, not shown in Table).
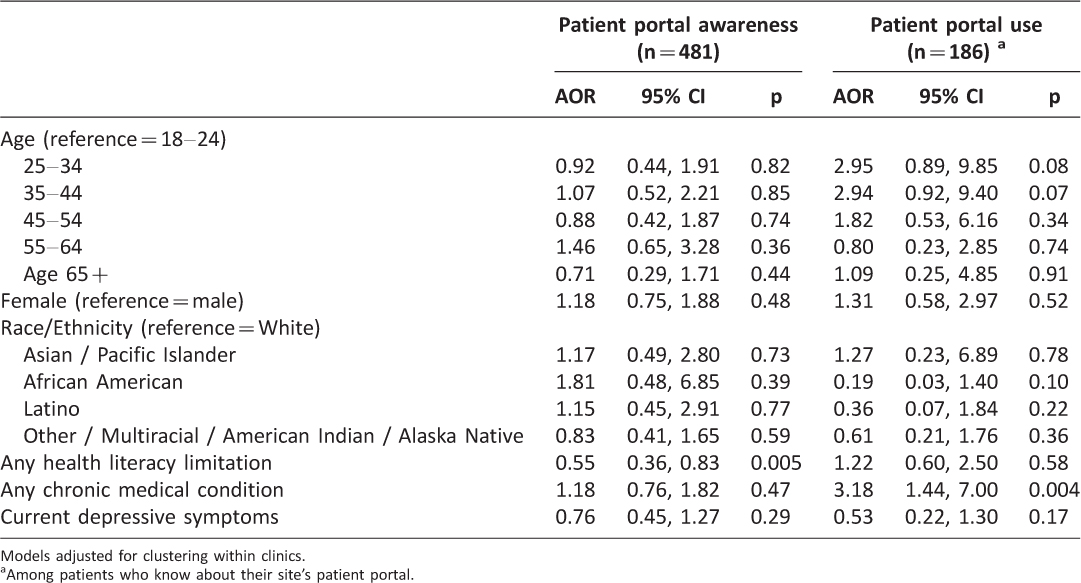
Table 3: Correlates of patient portal awareness and use among patients at 5 sites with a patient portal
Discussion
Although patient-facing HIT has only recently been introduced into healthcare delivery in the United States, our results demonstrate high acceptance by most patient groups. A majority of patients were comfortable sharing patient-reported mobile health data with healthcare providers and most patients who were aware of their clinic’s patient portal used it. Use of an electronic patient portal was particularly high among individuals with chronic diseases for whom timely communication with healthcare providers may be particularly valuable. However, attitudes and awareness were not uniformly positive and our findings reveal characteristics of patients and technologies that are associated with acceptability and use.
Importantly, older adults reported significantly less comfort with sharing patient-generated health data with healthcare providers, a finding that held in models that accounted for technology ownership. Although lower comfort in older adults thus cannot be attributed solely to lower technology ownership, the association did not persist once actual use of mobile health tools was accounted for. Given the cross-sectional nature of the survey, we cannot determine causality as use of mobile health tools may increase comfort with mobile data sharing, or comfort may precede use. Interestingly, older adults were equally likely as younger counterparts to be aware of their clinic’s patient portal and to use it, suggesting that age-associated patterns in technology attitudes and use differ across types of health technologies and platforms. Future research should be directed at understanding the factors that facilitate adoption of health technologies by the subgroup of older adults who report both comfort sharing mobile health data and use of mobile health tools. This research will inform efforts to encourage health technology use more broadly among older populations. We also note that young adults between 18 and 24 years of age were somewhat less likely than those between 25 and 44 years to use a patient portal. We speculate that this could reflect a general tendency in that age range to be less engaged with the healthcare system and suggest that future research should have a specific focus on health technology use among older adolescents as they transition into young adulthood.
Our findings contribute greater understanding to associations between health literacy limitations and HIT use. We found that health literacy limitations were associated with lower awareness of a clinic’s patient health portal. Future research should examine whether clinic staff or providers may be less likely to offer patient-facing technologies to patients with health literacy limitations. In contrast, health literacy limitations were not associated with comfort with mobile health data-sharing or with actual use of the patient portal among those who were aware of their clinic’s portal. Together these findings illustrate important nuances in understanding associations between health literacy and HIT use that are directly relevant for potential interventions. Past studies have documented that low awareness of patient-facing HIT represents a major barrier to patients’ use25–27 and therefore efforts to increase awareness of health technologies should explicitly target patients with health literacy limitations to address this barrier and mitigate potential disparities in health technology use.
We found that more patients were comfortable sharing mobile health data with providers than with third-party storage. This discrepancy may suggest that patients are more willing to use HIT that is offered directly by their healthcare system than through external vendors. Our survey did not assess this directly; however, this interpretation would be consistent with prior findings that patient-provider communication and trust in providers are associated with patients’ use of electronic portals.28 Although reported attitudes may be more conservative than actual behavior,29,30 we did find that comfort sharing mobile health data was strongly associated with actual use of a patient portal and therefore the discrepancy in attitudes may have implications for adoption. Conversely, it is possible that the item wording and the hypothetical nature of the questions led to more negative attitudes toward third-party involvement in mobile health data storage and that patients may be more willing to use third party tools when presented to them than their reported attitudes suggest. Future research should assess the robustness of these differences in patient preferences by including a more varied set of questions for comfort sharing with different recipients. Likewise, future research should assess how patients’ comfort may differ for different types of health data, particularly for information that may be considered sensitive, such as substance use, sexual behaviors, or mental health and to what extent individual differences exist in comfort for different types of information.
The present survey provides key information about patients’ attitudes and use of patient-facing health technologies, however certain limitations should be considered. The survey was conducted among individuals presenting for primary care appointments and therefore the sample may have been enriched in individuals who exhibit greater healthcare help-seeking. For example, depressed individuals use more primary care services than non-depressed counterparts, and therefore would have been more likely to be included in the sample. However, individuals with significant depression may have been less likely to participate due to low motivation. Notably, the percentage of individuals in our sample with significant depressive symptoms (21%) is similar to estimates of the prevalence of depression in primary care settings, suggesting minimal bias. The consumer market for mobile technologies has continued to evolve rapidly since the time that data collection occurred and it is likely that patients’ attitudes and use are also evolving, both as exposure to technologies increases and as reports of security concerns emerge.31,32 Our survey did not address patients’ use of wearable devices. Because these devices were less common when the survey was conducted and many such devices are connected to smartphone health apps, we suspect that the survey captured the majority of patients’ use of mobile health technologies at the time. The study was based on self-report measures of attitudes and use which may differ from observed use of health technologies. Finally, the survey did not assess patients’ beliefs about the value of HIT use for improving their health and well-being. Prior studies have suggested that evidence of efficacy is an important factor for patient adoption,26,33 yet studies to date have been inconsistent in identifying such benefits.27
This study highlights several practice implications. Efforts to disseminate patient-oriented technologies should include proactive patient education about new tools with a specific focus on increasing awareness among patients with health literacy limitations. Such efforts could also include components to educate patients regarding the privacy and security of their health data, particularly among older adults who endorse more concerns than younger counterparts. Past research has documented that healthcare providers play an important role in encouraging HIT use among their patients,26,27 and therefore efforts to promote patients’ use of HIT may also include education for providers to enhance providers’ “buy-in” and include strategies for providers to encourage patients’ adoption. Other strategies include providing hands-on guidance to patients to introduce them to the patient portal, for example by having a member of the clinic staff available to help patients enroll and learn to navigate it.
Healthcare is undergoing a significant transformation as patient portals are being deployed rapidly in the context of Meaningful Use incentives that require them and as integrating patient-reported outcomes into electronic health records is gaining momentum. Simultaneously, as more information technology companies develop and market health-related products and services, patients will have access to an expanding array of health technologies and may look to healthcare providers and systems for guidance in navigating these options. By increasing understanding of patient preferences, patterns of adoption, and barriers, healthcare systems will be better positioned to develop successful strategies to offer health technologies to their patients. Our results indicate a significant opportunity for increasing patient use of health information technologies by increasing awareness and educating patients about how systems protect the security of patient-reported health data. To mitigate disparities in care, such efforts should specifically target high priority groups such as older adults and those with health literacy limitations, while continuing to engage patients with chronic diseases.
Conflicts of Interest
The authors report no potential conflicts of interest.
Acknowledgements
The authors wish to thank the participating clinics, project champions, and patients for their valued contributions to this study. In addition, the authors acknowledge the recent loss of our coauthor Wayne J. Katon MD. Dr. Katon’s inspiration and guidance was instrumental to this research and we are deeply grateful to have had him as a member of our team. This project was supported by the Kaiser Permanente Northern California Community Benefit Program and the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number KL2TR000421 and grant UL1TR000423 through the Clinical and Translational Science Awards Program (CTSA). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
1. Steinhubl SR, Muse ED, Topol EJ. Can mobile health technologies transform health care? JAMA. 2013;310(22):2395–6. ![]()
2. Topol EJ, Steinhubl SR, Torkamani A. Digital medical tools and sensors. JAMA. 2015;313(4):353–4. ![]()
3. Steinhubl SR, Muse ED, Topol EJ. The emerging field of mobile health. Sci Transl Med. 2015;7(283):283rv283.
4. Pew Research Center. The Smartphone Difference. 2015; http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/. Accessed 8/18/15.
5. Workman B. The Explosion In Health Apps, And How They’re Disrupting The Gigantic, Lethargic Health Care Industry. Business Insider. 2013. http://www.businessinsider.com/mobile-will-disrupt-health-care-2013-9. Accessed 11/6/13.
6. Edelman. Edelman Trust Barometer Executive Summary. 2015: http://www.edelman.com/2015-edelman-trust-barometer-2/trust-and-innovation-edelman-trust-barometer/executive-summary/. Accessed 8/18/15.
7. DesRoches CM, Charles D, Furukawa MF, et al. Adoption of electronic health records grows rapidly, but fewer than half of US hospitals had at least a basic system in 2012. Health Aff (Millwood). 2013;32(8):1478–85. ![]()
8. Adler-Milstein J, DesRoches CM, Furukawa MF, et al. More than half of US hospitals have at least a basic EHR, but stage 2 criteria remain challenging for most. Health Aff (Millwood). 2014;33(9):1664–71. ![]()
9. Agaku IT, Adisa AO, Ayo-Yusuf OA, Connolly GN. Concern about security and privacy, and perceived control over collection and use of health information are related to withholding of health information from healthcare providers. J Am Med Inform Assoc. 2014;21(2):374–8. ![]()
10. Liu V, Musen MA, Chou T. Data breaches of protected health information in the United States. JAMA. 2015;313(14):1471–3. ![]()
11. Sarkar U, Karter AJ, Liu JY, et al. The literacy divide: health literacy and the use of an internet-based patient portal in an integrated health system-results from the diabetes study of northern California (DISTANCE). J Health Commun. 2010;15 Suppl 2:183–96.
12. Ancker JS, Barron Y, Rockoff ML, et al. Use of an electronic patient portal among disadvantaged populations. J Gen Intern Med. 2011;26(10):1117–23. ![]()
13. Goel MS, Brown TL, Williams A, Hasnain-Wynia R, Thompson JA, Baker DW. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med. 2011;26(10):1112–6. ![]()
14. Smith SG, O’Conor R, Aitken W, Curtis LM, Wolf MS, Goel MS. Disparities in registration and use of an online patient portal among older adults: findings from the LitCog cohort. J Am Med Inform Assoc. 2015;22(4):888–95. ![]()
15. Westfall JM, Zittleman L, Staton EW, et al. Card studies for observational research in practice. Ann Fam Med. 2011;9(1):63–8. ![]()
16. Bauer AM, Rue T, Keppel GA, Cole AM, Baldwin LM, Katon W. Use of mobile health (mHealth) tools by primary care patients in the WWAMI region Practice and Research Network (WPRN). J Am Board Fam Med. 2014;27(6):780–8. ![]()
17. Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–94.
18. Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23(5):561–6. ![]()
19. Sarkar U, Schillinger D, Lopez A, Sudore R. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. J Gen Intern Med. 2011;26(3):265–71. ![]()
20. Bauer AM, Schillinger D, Parker MM, et al. Health literacy and antidepressant medication adherence among adults with diabetes: the diabetes study of Northern California (DISTANCE). J Gen Intern Med. 2013;28(9):1181–7.
21. Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–92. ![]()
22. Lowe B, Kroenke K, Grafe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. 2005;58(2):163–71. ![]()
23. Fox SD, Maeve. Mobile Health 2012. Washington DC: Pew Research Center; 2012: http://pewinternet.org/Reports/2012/Mobile-Health.aspx. Accessed 5/12/2014.
24. Rubin D. Multiple Imputation for Nonresponse in Surveys. New York: Wiley; 1987.
25. Goel MS, Brown TL, Williams A, Cooper AJ, Hasnain-Wynia R, Baker DW. Patient reported barriers to enrolling in a patient portal. J Am Med Inform Assoc. 2011;18 Suppl 1:i8–12.
26. Amante DJ, Hogan TP, Pagoto SL, English TM. A systematic review of electronic portal usage among patients with diabetes. Diabetes Technol Ther. 2014;16(11):784–93. ![]()
27. Ronda MC, Dijkhorst-Oei LT, Rutten GE. Reasons and barriers for using a patient portal: survey among patients with diabetes mellitus. J Med Internet Res. 2014;16(11):e263.
28. Lyles CR, Sarkar U, Ralston JD, et al. Patient-provider communication and trust in relation to use of an online patient portal among diabetes patients: The Diabetes and Aging Study. J Am Med Inform Assoc. 2013;20(6):1128–31. ![]()
29. Barnes SB. A privacy paradox: Social networking in the United States. First Monday. 2006;11(9).
30. Norberg PA, Horne DR, Horne DA. The privacy paradox: Personal information disclosure intentions versus behaviors. J Consum Aff. 2007;41(1):100–26. ![]()
31. Powell AC, Landman AB, Bates DW. In search of a few good apps. JAMA. 2014;311(18):1851–2. ![]()
32. Huckvale K, Prieto JT, Tilney M, Benghozi PJ, Car J. Unaddressed privacy risks in accredited health and wellness apps: a cross-sectional systematic assessment. BMC Med. 2015;13(1):214. ![]()
33. Goldzweig CL, Orshansky G, Paige NM, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med. 2013;159(10):677–87. ![]()
Appendix. Mobile Technology and Health Survey Instrument
The survey was printed on both sides and folded in half to distribute it as a “booklet”.