An Affordable Smart Phone Communication System from Highway to Helipad: A Case Series
Jordan Koll1, Douglas Martin MD FRCP(C)2,3, Gregory Hansen MD FRCP(C) MPH MSc4
1Public Health Agency of Canada, Winnipeg, Manitoba, Canada; 2Department of Emergency Medicine, University of Manitoba, Health Sciences Centre, Winnipeg, Manitoba, Canada; 3Shock Trauma Air Rescue Society (STARS), Winnipeg, Manitoba, Canada; 4Divison of Pediatric Critical Care, University of Saskatchewan, Royal University Hospital, Saskatoon, Saskatchewan, Canada.
Corresponding Author: gregory.hansen@usask.ca
Journal MTM 8:1:53–60, 2019
Introduction: Improving communication between all providers involved with rural trauma and urgent care patients may be beneficial. In our proof of concept study, we examine the potential of an open architecture and flexible smart phone system, utilizing an affordable, off-the-shelf and secure application called Wickr.
Methods: Two patient scenarios were constructed to test the capabilities of the Wickr application for data transfer. Roles were distributed between three players: one represented the transport medical doctor, another played the air medical crew, and the final assumed all the other roles. As the two scenarios unfolded simultaneously, phone conversations, text messages, pictures, and imaging files were conducted between the players by smart phones via downloaded Wickr applications. Upon completion, players answered nine questions on a 5-point Likert scale that focused on the quality of the videos, texts and pictures shared, as well as indicators that we deemed essential to transport communication systems from our experience.
Results: Scores on video, picture and sound quality ranged from good to excellent. Scores on user friendliness, task suitability, speed, information discretion and customizable data retention ranges from somewhat agree to agree.
Conclusion: Wickr was quick, user friendly, and well suited for the clinical communication during simultaneous patient scenarios. Whether it is a capable system for a busy helicopter emergency medical service has not been evaluated.
Key Words: emergency medical services, mhealth, rural health, telemedicine, emergency care, Prehospital
Introduction
Over 46 million American and 7 million Canadian residents do not have access within 1-hour following injury to level I or level II trauma centers.1,2 Many others have medical conditions that require emergent and time-sensitive access to specialized treatment or diagnostics (i.e. acute ischemic stroke or myocardial infarction) available only at distant tertiary centers. Typically these patients are initially managed in rural, remote or isolated health centers, which may not have appropriate medical expertise or trauma resources. As poorer outcomes have been observed with rural trauma3,4 acute myocardial infarction,5–7 and prolonged time to definitive stroke treatment,8 improvements to pre trauma/tertiary hospital care should be considered.
Rural trauma and urgent care systems coordinate the initial emergency medical services (EMS) response, organize rapid transfers to smaller health centers, and quickly refer to trauma or tertiary centers when appropriate.2 Specialized retrieval teams within these systems have evolved over the past few decades,9 with the goal to improve care and expedite both scene and interfacility transports to the trauma or tertiary center. Evidence from recent military conflicts suggested that specialized trauma retrieval teams are effective and achieve improved survival outcomes.10,11 Data from the civilian context suggests similar benefits.12 While the optimal composition of the transport crew has not been established, improved outcomes may be further related to enhanced critical care training and experience.13
Rural trauma and urgent care systems have also utilized telecommunication technologies to improve patient care.14 In closed centralized models, medical control originates from a hub and is delivered to spoke rural centers or transport assets.15,16 This approach has facilitated management recommendations17 and improved interfacility care18 and clinical quality.19 However, significant limitations exist, including considerable expenses, vendor dependency, inability to involve non-spoke care providers, and inability for conference communication.15, 20
A telecommunication model for which trauma and urgent care expertise is available for all rural, EMS and transport crew providers may be beneficial. In our proof of concept study, we examine the potential of an open architecture and flexible smart phone system, utilizing an off-the-shelf application, with an emergency physician acting as the medical lead.
Methods
Wickr
Wickr Professional (Wickr Inc., San Francisco, USA) is an app (Figure 1) that enables participants using iOS and Android-based smart devices, MS Windows, and Mac OS computers to exchange end-to-end encrypted and content-expiring messages, photos, videos, and enable encrypted voice and video conferences (Figure 2). Wickr is an Internet-accessible electronic platform for exchanging personal health information that satisfies data sharing requirements in accordance with the Health Insurance Portability and Accountability Act (HIPAA) (Figure 3).3 It protects users of its network by storing a minimal quantity of identifiers in an encrypted, unrecoverable format, and data by utilizing advanced encryption algorithms and Perfect Forward Security to protect against compromises of message keys. For additional security – or if an organization requires it – Wickr can be hosted as an ‘on premise’ solution, installed and configured by an organization’s IT team.
Figure 1: Wickr secure login.
Figure 2: Wickr Options
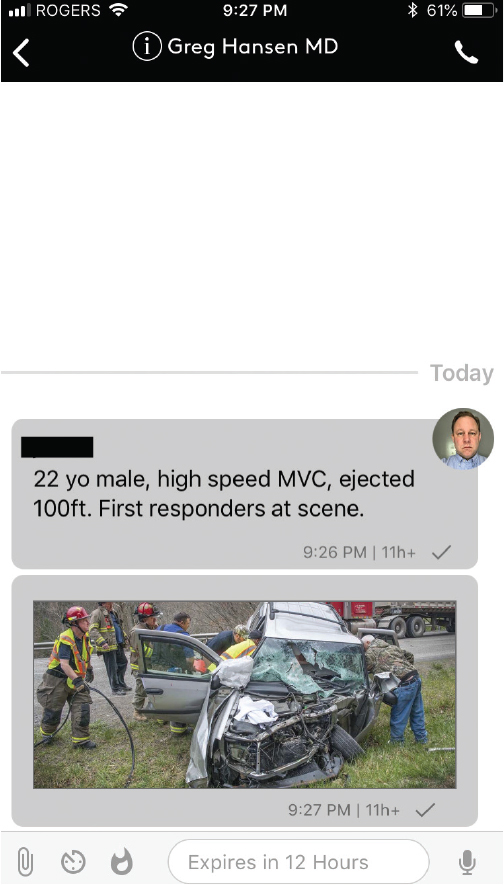
Figure 3: Wickr example of text message with photo and a timed deletion.
Wickr was selected as it has several advantages over telehealth and mobile communication systems tested or utilized by EMS organizations.22–26 These systems can have significant security issues that may not be accepted by current privacy regulatory standards. For this reason, by selecting Wickr our approach was to prioritize data security and privacy up front, with the understanding it is difficult to architect data security into solutions after the fact. Furthermore, their focus has been on software development and not processes, for the evolving pre-hospital patient. In contrast, our strategy has been to emphasize an open, interoperable communication platform to engage our team, and iterate our processes quickly versus waiting for software development resources to be available.
One of the authors (JK) had previously used Wickr Messenger, and a request for information led to an invite to participate in a private beta test of the enhanced professional version. For this proof of concept, we utilized Wickr’s Internet-accessible infrastructure and an early preview (alpha release) of Wickr Professional, as a smart phone communication system for sharing evolving patient information during two trauma transport scenarios.
Rural Trauma and Urgent Care System
Rural trauma within a 275 km concentric of Winnipeg, Canada are initially triaged through a provincial call center. The centre rapidly and simultaneously notifies both rural ground EMS and the specialized trauma helicopter EMS (HEMS) crew if the reported patient acuity is high. Depending on scene location, actual patient acuity and clinical trajectory, HEMS may be stood down, land at the scene, or retrieve the patient at a rural health center. The HEMS air medical crew (AMC) consists of a specialized registered nurse and an advanced care paramedic. A transport MD (medical doctor) provides online (real time) medical control from a central location if the team is utilized.
Trauma and Urgent Care Scenarios
Two scenarios (Figure 4) were created that included a 45-year old male with severe traumatic brain injury secondarily to a high speed motor vehicular collision, and a 55-year old male with acute onset of severe chest pain. Scenarios were constructed to model “real world” situations, which might test the capabilities of the Wickr application for data transfer using several different modalities and file sizes. Scenarios are not intended to be representative of ideal medical care.
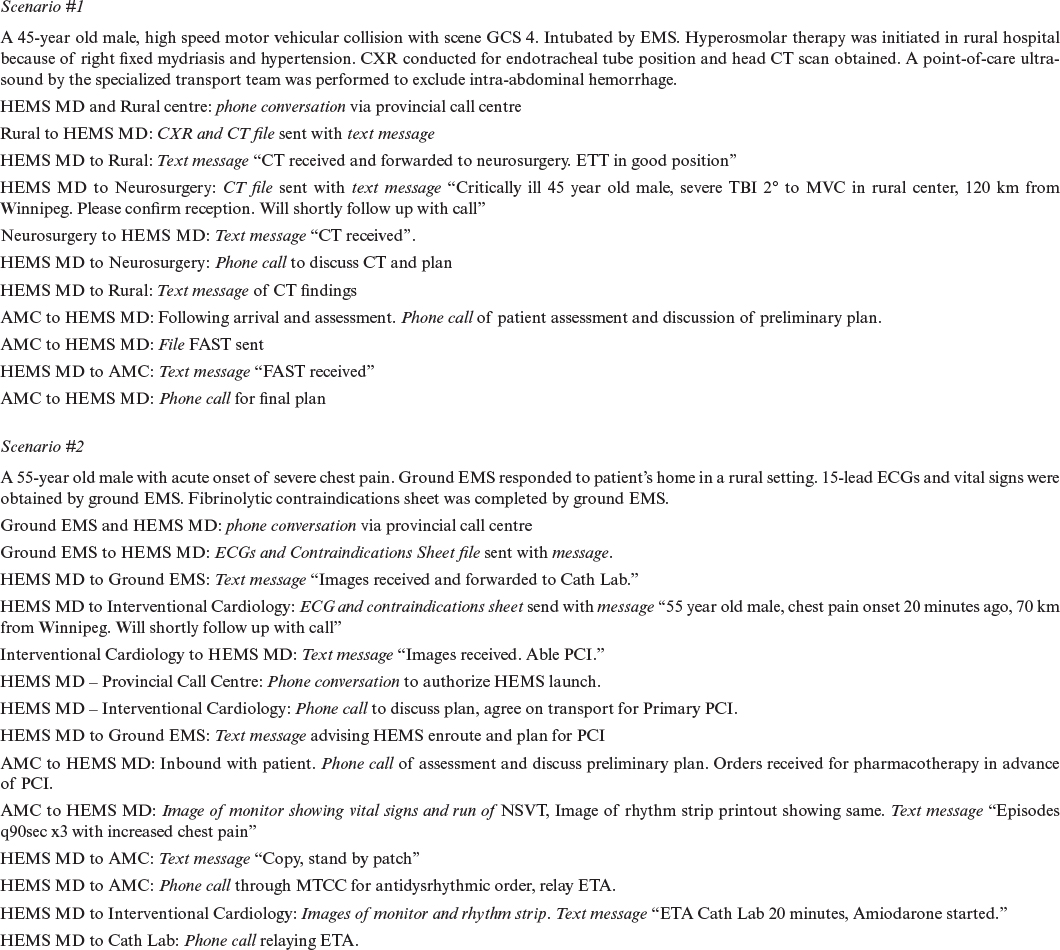
Figure 4: Clinical Scenarios with HEMS Medical Control
AMC – Air Medical Crew; CT – computed tomography; CXR – chest x-ray; ECG – electrocardiogram; EMS – Emergency Medical Service; ETA – Estimated Time of Arrival; ETT – endotracheal tube; FAST – Focused Assessment with Sonography in Trauma; GCS – Glasgow Coma Scale; HEMS MD – Helicopter Emergency Medical Services Medical Doctor; NSVT- Non-Sustained Ventricular Tachycardia; PCI – Percutaneous Coronary Intervention.
Roles were distributed between the three authors: one represented the transport MD (DM), another played the AMC (GH), and the final (JK) assumed all the other roles. Communication between the players was conducted by Apple iPhones and downloaded Wickr applications in an area with 3G/LTE coverage. Dialogue consisted of conversations, text messages, pictures, and imaging files. The two scenarios unfolded simultaneously via separate initiating calls from the mock provincial call centre, followed by sequential actions coordinated by the transport MD. The electrocardiogram, chest roentgenogram, and head computed tomography images were found in the public domain (Creative Commons CCO 1.0 Universal Public Domain Dedication, Wikimedia Commons). The shared focused assessment with sonography in trauma was an author’s (DM) personal scan for this project, and the monitor image came from our simulation lab.
Metrics
All three authors answered nine questions on a 5-point Likert scale (1 “disagree” to “unacceptable” to 5 “agree” or “excellent”) upon completion of the scenarios. The questions focused on the quality of the videos, texts and pictures shared, as well as indicators that we deemed essential to transport communication systems from our experience. This included whether the system, 1) was intelligible to the new user (“User Friendliness”); 2) was well matched to the situational requirements of clinical communication (“Task Suitability”); 3) allowed the required communication to occur without fault or interruption (“Reliability”); 4) allowed for timely communication (“Speed”); 5) allowed the user to discriminate which information is shared with other parties; (“Information Discretion”) and, 6) could preferentially archive, erase or export all aspects of the communication (“Customizable Data Retention”). Due to the small sample size, raw data was documented only.
Results
Likert scores between the three authors varied by one or less for all indicators (Table 1). Video, picture and sound quality ranged from good to excellent (Likert 4 and 5). The Wickr system also received Likert 4 and 5 scores (somewhat agree to agree) on user friendliness, task suitability, speed, information discretion and customizable data retention. Reliability received the lowest scores (2,3,3).
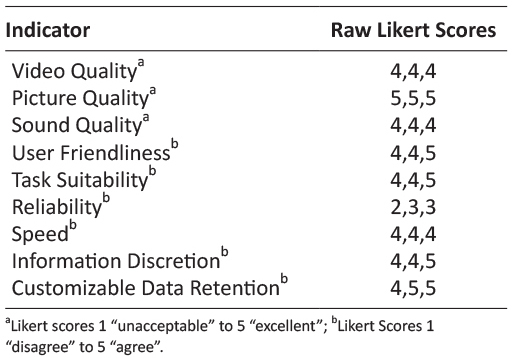
Table 1: Wickr Pilot Evaluation
Discussion
The purpose of this proof of concept study was to examine the potential of an off-the-shelf smart phone app as a medical telecommunication system for a HEMS program. By activating two simultaneous and scripted trauma team scenarios, we found that Wickr was quick, user friendly, provided appropriate discretion and control over health information, and was well suited for the clinical communication and archiving requirements of a trauma transport program. Its advantages over centralized hub and spoke models may include cost, customizability, ability to add consultants to a call, and mobility of the transport MD. Its major disadvantage includes potentially suboptimal telecommunication coverage maps.
The Wickr system was intelligible to the authors who were all novices with the app. A very brief orientation to the system was provided at the onset of the scenarios, but its interface resembled a default iPhone or Android messaging app and consequently became quickly familiar. Capturing images and videos, making voice and video calls, and attaching media to messages were analogous to how smart devices are used for personal communication.
The Wickr system was well suited for the clinical communication requirements of a HEMS program. First, the transport MD had complete control over who received information, and for how long secure messaging could be accessed prior to deletion. This is an important asset to quality reviews, as the system can archive aspects of a patient transport that may otherwise be undocumentable. Just as importantly, the information technology (IT) team or administrator can control how long (by policy) recipients have access to any message by specifying a time to “live”. For example, if a snapshot of a patient’s roentgenogram was shared, the transport MD’s Wickr app can destroy the keys required for decryption, allowing for deletion from the device, and ensuring the image cannot be recovered. Second, the transport MD was not constrained to a central console, allowing for enhanced mobility to address other professional tasks when not directly involved in patient care. Finally, with a focus on workflow and not features, the transport MD could easily manage two simultaneous scenarios, and smoothly navigate around communication from the AMCs, referring MDs and consultants. Wickr allowed for both peer to peer messaging, as well as the ability to establish secure ‘chat rooms’ that allow multiple participants to have real time access to text, photo, video data and the ability to participate in up to 10 way voice and video calling. This capacity to add novel or known consultants and referring MDs to the system while a clinical scenario evolves may be advantageous over traditional hub and spoke models, which are vendor restricted and difficult to customize in a timely manner.27,28
Perhaps Wickr’s greatest advantage over centralized vendor solutions is cost. Although the tested Wickr Professional is not publicly available, our understanding is that it will be offered at around $25 US/seat for the software as a service (SaaS) model, with the benefit of decoupling licenses from devices (accessed on multiple devices by the licensed user), and avoiding capital costs of licensing and hardware refreshing. Improvement in technology and features also occur on an annual basis for the same price (i.e. a wireless and data plan). Although BYOD offers similar advantages to Wickr from the standpoint of costs, built in messaging apps should always be considered insecure. This not only pertains to the transmission of data, but also because there is no segregation between personal and confidential patient data on the smart device itself. Regardless, BYODs with a multitude of apps continue to be employed as ad hoc communication platforms, despite the awareness of potential security concerns.29 It is important to note that while Wickr’s level of data security safeguards Personal Health Information, untangling the web of policy and legislation that health jurisdictions may require to implement such a system may nonetheless be challenging.30 Constraints placed on the in-flight operation of Personal Electronic Devices (PEDs) by aviation regulatory bodies may represent a second source of challenge to a smartphone based medical communication system.31
The strength of centralized hub and spoke models has been their reliance on a series of fixed, leased telecommunication lines that guarantee with a degree of certainty the quality and availability of connections. Wickr or BYOD solutions however, offer a trade-off of this certainty in return for flexibility and mobility. In our testing we initially experienced some challenges, as one of the author’s device’s intermittently ‘froze’ when connecting to the Wickr network. However, we were unable to determine whether this was a device issue (iPhone 5 versus 6s) or with the pre-production software release. It is understood that encryption adds some overhead to communication, and Wickr is currently addressing this matter. Furthermore, by relying on cellular wireless data networks, Wickr’s reliability and speed of data transmission can be predicted on the coverage map of telecommunication providers operating in a jurisdiction. With the assistance from Wickr, we conducted a basic network test to capture network provider, network and signal strength in a representative rural service area within the HEMS catchment. While connected to a high speed (LTE) network with the weakest (-118 dBa) to the strongest (-90 dBa) being recorded, we were able to consistently send and receive secure communications from Wickr on the other end. LTE network coverage was available from the helipad or parking areas of rural health facilities, although rural highways were a mix of LTE and slower, 3G connections. In areas where LTE was not available, future testing may consider the use of portable cellular signal boosters to improve connectivity.
Practically, Wickr should not be viewed as a substitute for a bedside evaluation. Critical elements of the patient exam (i.e. heart and lung sounds) obviously cannot be appreciated with the app, and must be assimilated into the context of the patient’s clinical trajectory. With hyperacute patient presentations requiring immediate attention, the use of Wickr during these stressful times may not be intuitive or safe. On the surface, utilizing Wickr may appear superior to standard phone discussions, through its ability to provide real time visual information that can be safely and easily shared with multiple health providers. However, communication patterns with several consultants in a private chat room have to yet be clearly defined, and are a fascinating area of research. How to manage competing interests, membership to the chat room (inclusion/exclusion) and leadership of the discussion, are only a few of the potential hot spots that may require deft navigation.
Our study had several limitations. First, to reflect typically HEMS volume, the Wickr system was trialed with two simultaneous trauma team scenarios. However, given its ease of use, it is unlikely that more scenarios or other acute presentations i.e. acute respiratory failure, toxidrome, would have added further layers of complexity. Second, the sample size of three evaluations was very small, and consequently carried a high bias risk. Nevertheless, we are confident that our proof of concept study was able to demonstrate Wickr’s telecommunication potential for a larger scale assessment.
Conclusions
Effective telecommunication technologies for HEMS programs managing rural trauma are vital for optimal patient management. Our proof of concept study was able to demonstrate that Wickr, an open architecture, flexible and HIPAA compliant smart phone communication system, was quick, user friendly, and well suited for the clinical communication during simultaneous mock trauma scenarios. Whether it is effective on a large scale has yet to be established.
Compliance with Ethical standards
Funding
Authors have not received any funding nor financial incentives for this study.
Conflict of Interest
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
References
1. Branas CC, Mackenzie EJ, Williams JC, et al. Access to trauma centers in the United States. JAMA 2005; 293(21): 2626–2633. doi:10.1001/jama.293.21.2626 ![]()
2. Hameed SM, Shuurman N, Razek T, et al. Access to trauma systems in Canada. J Trauma 2010; 69(6): 1350–1361. doi: 10.1097/TA.0b013e3181e751f7 ![]()
3. Grossman DC, Kim A, MacDonald SC, et al. Urban-rural differences in prehospital care in major trauma. J Trauma 1997; 42(4): 723–729. ![]()
4. Muelleman RL, Wadman MC, Tran TP, et al. Rural motor vehicle crash risk of death is higher after controlling for injury severity. J Trauma 2007; 62(1): 221–226. doi 10.1097/01.ta.0000231696.65548.06 ![]()
5. Bhuyan SS, Wang Y, Opoku S, et al. Rural-urban differences in acute myocardial infarction mortality: evidence from Nebraska. J Cardiovasc Dis Res 2013; 4(4): 209–213. doi: 10.1016/j.jcdr.2014.01.006
6. Nawal Lutfiyya M, Bhat DK, Gandhi SR, et al. A comparison of quality of care indicators in urban acute care hospitals and rural critical access hospitals in the United States. Int J Qual Health Care 2007; 19(3): 141–149. doi: 10.1093/intqhc/mzm010 ![]()
7. Baldwin LM, MacLehose RF, Hart LG, et al. Quality of care for acute myocardial infarction in rural and urban US hospitals. J Rural Health 2004; 20(2): 99–108. ![]()
8. Saver JL. Time is brain–quantified. Stroke 2006; 37(1): 263–266. doi: 10.1161/01.STR.0000196957.55928.ab ![]()
9. Droogh JM, Smit M, Absalom AR, et al. Transferring the critically ill patient: are we there yet? Crit Care 2015; 19(1): 62. doi: 10.1186/s13054-015-0749-4 ![]()
10. Apodaca A, Olson CM Jr, Bailey J, et al. Performance improvement evaluation of forward aeromedical evacuation platforms in Operation Enduring Freedom. J Trauma Acute Care Surg 2013; 75(2 Suppl 2): S157–S163. doi: 10.1097/TA.0b013e318299da3e ![]()
11. Ingalls N, Zonies D, Bailey JA, et al. A review of the first 10 years of critical care aeromedical transport during Operation Iraqi Freedom and Operation Enduring Freedom: the importance of evacuation timing. JAMA Surg 2014; 149(8): 807–813. doi: 10.1001/jamasurg.2014.621 ![]()
12. McVey J, Petrie DA, Tallon JM. Air Versus Ground Transport of the Major Trauma Patient: A Natural Experiment. Prehosp Emerg Care 2010; 14(1): 45–50. doi: 10.3109/10903120903349788 ![]()
13. Mabry RL, Apodaca A, Penrod J, et al. Impact of critical care-trained flight paramedics on casualty survival during helicopter evacuation in the current war in Afghanistan. J Trauma Acute Care Surg 2012; 73(2 Suppl 1): S32–S37. doi: 10.1097/TA.0b013e3182606001. ![]()
14. Perednia DA, Allan A. Telemedicine technology and clinical applications. JAMA 1995; 273(6): 483–488. ![]()
![]()
15. Reynolds HN, Bander JJ. Options for tele-intensive care unit design: centralized versus decentralized and other considerations. It is not just a “Another Black Sedan”. Crit Care Clin 2015; 31(2): 335–350. doi: 10.1016/j.ccc.2014.12.010 ![]()
16. Bjorn P. Rural teletrauma: applications, opportunities, and challenges. Adv Emerg Nurs J 2012; 34(3): 232–237. doi: 10.1097/TME.0b013e31825f6237 ![]()
17. Moya M, Valdez J, Yonas H, et al. The impact of a telehealth web-based solution on neurosurgery triage and consultation. Telemed J E Health 2010; 16(9): 945–949. doi: 10.1089/tmj.2010.0044 ![]()
18. Yperzeele J, Van Hooff RJ, De Smedt A, et al. Feasibility of AmbulanCe-based Telemedicine (FACT) study; safety, feasibility and reliability of third generation in-ambulance telemedicine. PLoS One 2014; 9(10): e110043. doi: 10.1371/journal.pone.0110043 ![]()
19. Mueller KJ, Potter AJ, MacKinney AC, et al. Lessons from tele-emergency: improving care quality and health outcomes by expanding support for rural care systems. Health Aff (Millwood) 2014; 33(2): 228–234. doi: 10.1377/hlthaff.2013.1016 ![]()
20. Merchant KAS, Ward MM, Mueller KJ, et al. Hospital views of factors affecting telemedicine use. Rural Policy Brief Apr 2015; (2015 5): 1–4.
21. Wickr. Is Wickr HIPAA, FIPS and NSA Suite B compliant [Internet]? 2016 [cited 2017 Feb 2]. Available from: https://wickr.desk.com/customer/en/portal/articles/2341613-is-wickr-hipaa-fips-and-nsa-suite-b-compliant-.
22. Xiao Y, Gagliano D, LaMonte M, et al. Design and evaluation of a real-time mobile telemedicine system for ambulance transport. J High Speed Network 2000; 9(1), 47–56.
23. Chan AT. WWW+ smart card: towards a mobile health care management system. Int J Med Inform 2000; 57(2): 127–137. ![]()
24. Chu Y, Ganz A. A mobile teletrauma system using 3G networks. IEEE Trans Inf Technol Biomed 2004; 8(4): 456–462. ![]()
25. Abed Y, Schooley B, Murad A, et al. Using a Mobile Multimedia System to Improve Information Exchange in EMS. AMCIS 2012 Proceedings 2012; 28.
26. Schooley B, Abed Y, Murad A, et al. Design and field test of an mHealth system for emergency medical services. Health Tech 2013; 3(4): 327–340.
27. Raths D. Behind Intermountain’s Build-or-Buy Decision on Telehealth Platform [Internet]. 2014 [cited 2017 Feb 1]. Available from: http://www.healthcare-informatics.com/article/behind-intermountain-s-build-or-buy-decision-telehealth-platform. ![]()
28. Geiger G. Mobile technology takes The Ottawa Hospital further on its journey toward excellence. Advocate 2011; 18(3): 5–6.
29. Koehler N, Vujovic O, McMenamin C. Healthcare professionals’ use of mobile phones and the internet in clinical practice. JMTM 2013; 2(1). doi: 10.7309/jmtm.2.1.2. ![]()
30. Koll J, Hansen G. Mobile solutions for physicians shackled by electronic medical records. JMTM 2015; 4(3): 32–34. doi: 10.7309/jmtm.4.3.6
31. Transport Canada. Advisory Circular: Use of transmitting and non-transmitting portable electronic devices [Internet]. 2014 [cited 2016 Feb 1]. Available from: https://www.tc.gc.ca/media/documents/ca-opssvs/ac-700-005.pdf. ![]()

