REST – An Innovative Rapid Eye Screening Test
Chan Jan-Bond1, Teh Wee-Min1, Ng Hong-Kee1, Ik Zu-Quan2, Sonny-Teo Khairy-Shamel1, Embong Zunaina1, Ahmad-Tajudin Liza-Sharmini1
1Department of Ophthalmology, School of Medical Sciences, Universiti Sains Malaysia, Kubang Kerian, Kelantan, Malaysia; 2Department of Computer Science and Networked System, Faculty of Science and Technology, Sunway University, Bandar Sunway, Selangor, Malaysia
Corresponding author: janbond@hotmail.com
Journal MTM 4:3:20–25, 2015
Objectives: To determine the agreement and correlation of visual acuity between Rapid Eye Screening Test (REST) app and Early Treatment Diabetic Retinopathy Study (ETDRS) tumbling ‘E’ chart.
Methods: A visual acuity tool was designed for Android and iOS users based on ETDRS. A pilot study was conducted involving 101 subjects. Visual acuity of each subject was tested using ETDRS chart and crossover to REST at 3 meters or vice versa.
Results: Mean visual acuity using ETDRS was 0.086 ± 0.194 for right eye (RE) and 0.085 ± 0.196 for left eye (LE) while REST measurement was 0.091 ± 0.182 for RE and 0.098 ± 0.203 for LE. There was significant and strong direct correlation between visual acuity using ETDRS and REST in both eyes (RE: r = 0.829; p < 0.001, LE: r = 0.871; p < 0.001). The 95% limits of agreement between the two charts was ±0.11 LogMAR for right eye and ±0.10 LogMAR for left eye. Time taken for REST was significantly shorter than ETDRS (p < 0.001).
Conclusion: REST is accurate and time-saving, thus potentially ideal for mass screening in remote area.
Introduction
Community vision screening plays an important role in the detection of eye diseases, with the hope of early detection and prevention of potentially reversible causes of blindness. Approximately 285 million people have visual impairment worldwide, according to World Health Organization (WHO) estimates. Out of this, 90% of the visually impaired live in low-income settings1. In the community setting, healthcare workers usually perform visual acuity testing with a variety of tools such as Snellen chart2 and Early Treatment Diabetic Retinopathy Study (ETDRS) tumbling ‘E’ chart3, which have been validated4,5.
A wide range of products and greater affordability of digital devices such as smartphones and tablet computers have made these devices ubiquitous. Various innovations have been created to take advantage of these devices for the screening of eye diseases6, capturing of high-quality images of the eye7, or as an indispensable tool in patient education. Applications (or apps in short) created for these devices are convenient to use and can be easily downloaded. We are introducing an app called Rapid Eye Screening Test (REST) that is easily downloadable, and simple to use.
The purpose of this study was to determine the agreement and correlation of our REST app in com-parison with the standard ETDRS tumbling ‘E’ chart.
Methods
Development of REST
The REST app (Fig. 1) was written using HTML5 coding and is available for free on both Android and iOS operating system (OS) platforms for both smartphones and Ipads/Android tablets as well (downloadable from Google Play and App Store respectively) (Fig. 2). The tumbling E chart is recreated in the app and the optotype size is calibrated according to the testing distance of either 1 metre or 3 metres. The touchscreen function in these devices plus the addition of sound cues in the app allow for the tester to perform testing without having to look at the screen.

Figure 1: Screenshot of REST app
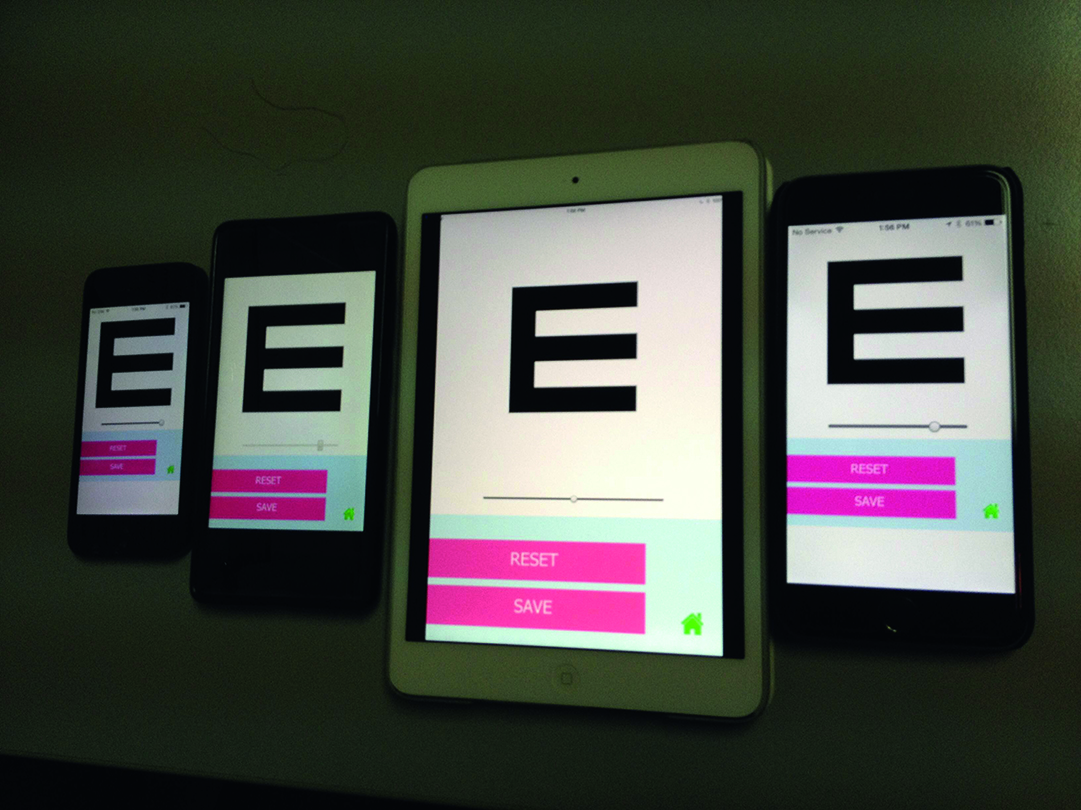
Figure 2: REST app across platforms (From Right: iPhone 5s, Xiaomi Redmi Note, iPad Mini 2, iPhone 6 Plus)
Calibration of the REST app
An initial calibration of the REST app needs to be done prior to initial use. On the main screen, user needs to click on the “Settings” tab. An option of 3 meters and 1 meter will be displayed and both need to be set. With the help of a ruler, the letter E displayed on the phone screen needs to be measured to 43 mm for 3 meters and 14 mm for 1 meter by sliding the toggle just below the E (Figure 3). Once the setting is done, user needs to click on save and the memory of the optosizing will be saved.
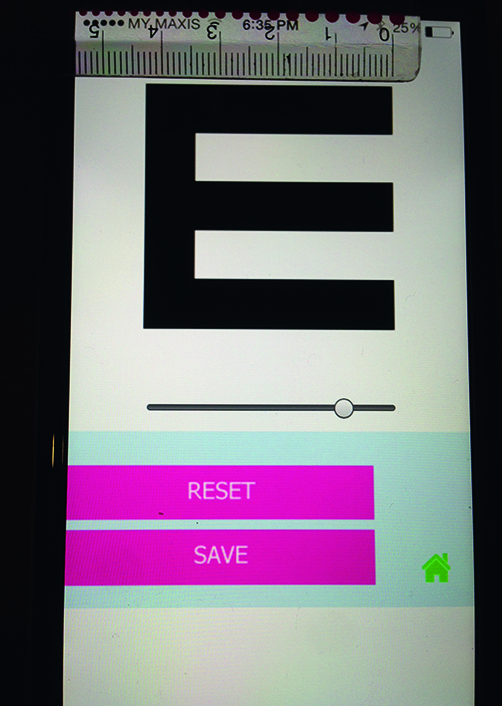
Figure 3: Initial setting of REST app
Instructions on how to use the REST app
The tester holds the smartphone or tablet at the preferred testing distance (either 1 or 3 meters) from the subject. Testing is done under normal lighting conditions and the device brightness is set to its highest setting. The subject is instructed to point with fingers to indicate the direction of the tumbling ‘E’ shown on the device. The tester then swipes accordingly. If the correct answer is given, a positive sound is played and the test proceeds to a smaller ‘E’. The test continues to reach a vision of 6/6 and a different positive sound will be played indicating end of testing. If the subject indicates a wrong direction anytime during the test i.e. the tester swipes to the wrong direction on the touchscreen, a negative sound will be played and the final vision will be displayed.
REST as Screening Tool
The video links to example of how REST is used as a screening tool.
Link: https://youtu.be/oWOP4wbB_J0
Pilot Study: Comparison between REST and ETDRS tumbling ‘E’ chart
This was a cross-sectional study employing universal sampling conducted in Universiti Sains Malaysia Hospital, a tertiary eye referral centre in the east coast of Malaysia. The study was conducted throughout the month of November 2014.
Study subjects comprised patients who attended the eye clinic and staff in the eye clinic at Hospital Universiti Sains Malaysia. Subjects with visual acuity of worse than 6/60 were excluded from the study. Visual acuity screening was performed sequentially in both eyes using the ETDRS tumbling ‘E’ chart at 3 meters, followed by the REST app at the same distance. The time taken for both tests to be completed and the final visual acuity were recorded. Demographics data of age, sex, race, highest education level, and nature of occupation were obtained from the subjects.
Visual acuity was then converted to logMAR (Minimal Angle of Resolution) for data analysis. Data analysis was done using SPSS software version 22.0. The intra-class correlation coefficient (ICC) was used to assess the test-retest reliability of the REST app and ETDRS tumbling ‘E’ chart. The Bland-Altman comparison method was used to assess agreement between the two methods. Pearson Correlation was used to determine the correlation while paired t-test was used to compare the time taken. A p value <0.05 was deemed statistically significant.
Results
A total of 101 subjects were recruited in this study. Mean age was 37.0 ± 15.9 years (range: 5.0–75.0 years). There were slightly more females (55.4%) compared to males. Majority of our subjects (62.4%) were Malays, followed by Chinese (31.7%) and Indians (5.9%), generally reflecting the racial distribution of the Malaysian population.
Most of our subjects (54.5%) had tertiary education, while 34.6% had secondary level education, 7.9% had primary education, while 3.0% had no formal education. Of the total of 101 subjects, 50.5% of the subjects were working professionals (doctors, nurses, optometrists), while 28.7% were non-professionals. The remaining 20.8% of subjects were unemployed.
In the standard ETDRS tumbling ‘E’ chart, the mean logMAR visual acuity was 0.086 ± 0.194 for the right eye and 0.085 ± 0.196 for the left eye. Meanwhile, the mean logMAR visual acuity for REST was 0.091 ± 0.182 for the right eye and 0.098 ± 0.203 for the left eye.
The ICC was found to be 0.905 (95% CI from 0.859 to 0.936, p <0.001) for right eye and 0.931 (95% CI from 0.898 to 0.954, p<0.001) for left eye. The extent of agreement between REST app and ETDRS tumbling ‘E’ chart is illustrated on Figure 4A and 4B. The 95% limits of agreement between the two charts were between +0.10 and −0.15 for right eye and +0.10 and −0.30 for left eye. There was strong direct correlation between visual acuity using ETDRS tumbling ‘E’ chart and REST in both eyes (right eye: r = 0.829; p < 0.001, left eye: r = 0.871; p < 0.001) (Figure 5 and Figure 6). The time taken to perform ETDRS tumbling ‘E’ chart and REST visual acuity examination is shown in (Table 1). The results showed that the time taken for REST was 2.8 ± 2.8 seconds shorter than ETDRS tumbling ‘E’ chart in the right eye and 3.0 ± 2.7 seconds shorter in the left eye. Both were statistically significant with p < 0.001.

Figure 4: Bland-Altman plot for difference in LogMAR visual acuity of right eye (A) and left eye (B) between REST app and ETDRS tumbling ‘E’ chart. In each instance, the mean difference and upper and lower 95% limits of each agreement are plotted.

Figure 5: Correlation of right eye vision between ETDRS tumbling ‘E’ chart and REST

Figure 6: Correlation of left eye vision between ETDRS tumbling ‘E’ chart and REST

Table 1: Comparison of time taken between ETDRS tumbling ‘E” chart and REST
Discussion
Visual acuity testing is an important first step in detecting reversible causes of visual impairment such as cataract and refractive errors8,9. In screening of large general population, a screening tool should be affordable to acquire, highly portable, and easy to use.
There is a variety of visual acuity screening tools in the market currently, including digital versions available as apps. However, one major shortcoming is the lack of ability to standardise or adjust the size of the optotype according to different testing distances. To our knowledge, at the time of writing, there is no paper published that studied the agreement and correlation between these visual acuity testing apps and the standard charts already available in the market.
In our study, we found that there was a strong direct correlation between REST and ETDRS tumbling ‘E’ chart as a visual acuity screening tool. The time taken to perform the test was significantly shorter compared to ETDRS tumbling ‘E’chart.
There are, however, limitations to our app. The screen contrast and brightness of the various touch-screen devices cannot be standardised due to the different builds and models. In addition, for our app to display properly, a minimum screen size of 3.5 inches (e.g. the screen size of an iPhone 4) is required. This is required due to the size of the optotype.
As our REST app is run on digital devices, it is highly reliant on the battery lifespan of each indi-vidual device. Nevertheless, this can be overcome by plugging the device into a power source.
Conclusions
The REST app is a potentially ideal app for visual acuity assessment in the general population, especially in remote areas where access to healthcare facilities may prove difficult. Its compact portability, ease of use and intuitive testing method offer users a rapid yet accurate means of testing visual acuity.
References
1. WHO. World Health Organization-Visual impairment and blindness factsheet2014 22 October 2014 22 October 2014]. Available from: http://www.who.int/mediacentre/factsheets/fs282/en/.
2. McGraw P, Winn B, Whitaker D. Reliability of the Snellen chart. Bmj. 1995;310(6993):1481–2. ![]()
3. Ferris FL, 3rd, Kassoff A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. American journal of ophthalmology. 1982;94(1):91–6. ![]()
4. Kuo HK, Kuo MT, Tiong IS, Wu PC, Chen YJ, Chen CH. Visual acuity as measured with Landolt C chart and Early Treatment of Diabetic Retinopathy Study (ETDRS) chart. Graefe’s archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2011;249(4):601–5. ![]()
5. Engin O, Despriet DD, van der Meulen-Schot HM, Romers A, Slot X, Sang MT, et al. Comparison of optotypes of Amsterdam Picture Chart with those of Tumbling-E, LEA Symbols, ETDRS, and Landolt-C in non-amblyopic and amblyopic patients. Graefe’s archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2014.
6. Vaughan J, editor Photoscreening for Refractive Error and Strabismus With a Smartphone App. 2013 AAP National Conference and Exhibition; 2013 26–29 October 2013; Orlando, Orange County Convention Center: American Academy of Pediatrics.
7. Chan JB, Ho HC, Ngah NF, Hussein E. DIY-Smartphone Slit-Lamp adaptor. Journal of Mobile Technology in Medicine. 2014;3(1):16–22. ![]()
8. Wang F, Tielsch JM, Ford DE, Quigley HA, Whelton PK. Evaluation of screening schemes for eye disease in a primary care setting. Ophthalmic epidemiology. 1998;5(2):69–82. ![]()
9. Quigley HA, Park CK, Tracey PA, Pollack IP. Community screening for eye disease by laypersons: the Hoffberger program. American journal of ophthalmology. 2002;133(3):386–92. ![]()
Appendix
Link to App:
Playstore: https://play.google.com/store/apps/details?id=com.mycompany.rest&hl=en

